MAO Inhibitors: Dangerous Interactions with Common Medications

MAO inhibitors are one of the oldest classes of antidepressants, but they’re also among the most dangerous if used incorrectly. Unlike newer antidepressants like SSRIs, MAOIs don’t just tweak brain chemistry-they fundamentally change how your body processes a wide range of substances. Even a single over-the-counter cold pill or a slice of aged cheese can trigger a life-threatening reaction. Despite their declining use, MAOIs are still prescribed today for treatment-resistant depression, and the risks haven’t changed. If you’re taking one-or know someone who is-understanding these interactions isn’t optional. It’s a matter of survival.
How MAO Inhibitors Work (and Why That’s Dangerous)
MAOIs block an enzyme called monoamine oxidase, which normally breaks down neurotransmitters like serotonin, norepinephrine, and dopamine. By preventing their breakdown, these drugs boost mood. But that same mechanism means your body can’t clear other substances either-especially those that also increase these same chemicals. When you combine MAOIs with certain medications, supplements, or even foods, neurotransmitter levels can skyrocket. That’s when things go wrong.
The two biggest dangers are hypertensive crisis and serotonin syndrome. Hypertensive crisis happens when tyramine-a compound found in aged and fermented foods-builds up because MAOIs can’t break it down. Tyramine forces your body to release massive amounts of norepinephrine, causing blood pressure to spike. Cases have been documented where systolic pressure jumped over 200 mmHg within an hour. Serotonin syndrome is even more unpredictable. Too much serotonin in the brain can cause seizures, fever above 106°F, muscle rigidity, and organ failure. Mortality rates for severe cases range from 2% to 12%.
Medications That Can Kill You When Taken With MAOIs
There are dozens of common medications that are absolute no-gos with MAOIs. Some you might never guess are dangerous.
- Dextromethorphan - Found in more than 100 cough syrups and cold remedies. A single 30mg dose in someone on phenelzine has triggered severe agitation, hyperthermia, and hospitalization. The FDA issued a warning in 1992, and it’s still not always clearly labeled.
- Tramadol, meperidine, methadone - These opioids are linked to serotonin syndrome. A 32-year-old man on selegiline ended up intubated after taking 50mg of tramadol. He survived, but many don’t.
- Linezolid - An antibiotic prescribed for stubborn infections. It’s also an MAOI. Taking it with another MAOI can cause fatal serotonin syndrome. The FDA added it to the contraindicated list in 2006 after multiple deaths.
- Phenylephrine - The active ingredient in many OTC decongestants like Sudafed PE. It directly raises blood pressure, and MAOIs make it worse. A 2022 study in the Journal of Clinical Psychiatry called this one of the most common causes of preventable MAOI-related emergencies.
- SSRIs and SNRIs - Fluoxetine (Prozac), sertraline (Zoloft), venlafaxine (Effexor). Combining these with MAOIs can cause serotonin syndrome within hours. The FDA requires a 14-day washout period between them. For fluoxetine, it’s 5 weeks because its metabolites stick around for months.
Supplements You Didn’t Know Were Risky
People assume natural means safe. That’s not true with MAOIs.
- St. John’s Wort - A popular herbal antidepressant. It increases serotonin. When taken with MAOIs, it’s a recipe for serotonin syndrome. A 2018 case report described a patient with a temperature of 40.5°C after combining it with phenelzine.
- 5-HTP - Sold as a sleep or mood aid. It’s a direct precursor to serotonin. Just 200mg with an MAOI can trigger a hypertensive crisis and serotonin syndrome simultaneously.
- SAMe - Often used for joint pain or depression. It boosts serotonin and dopamine. The American Psychiatric Association explicitly warns against its use with MAOIs.
- Ginseng - A 1985 case report linked ginseng to mania and tremors in someone on phenelzine. Researchers suspected caffeine contamination, but the risk remains unproven-and too dangerous to gamble on.

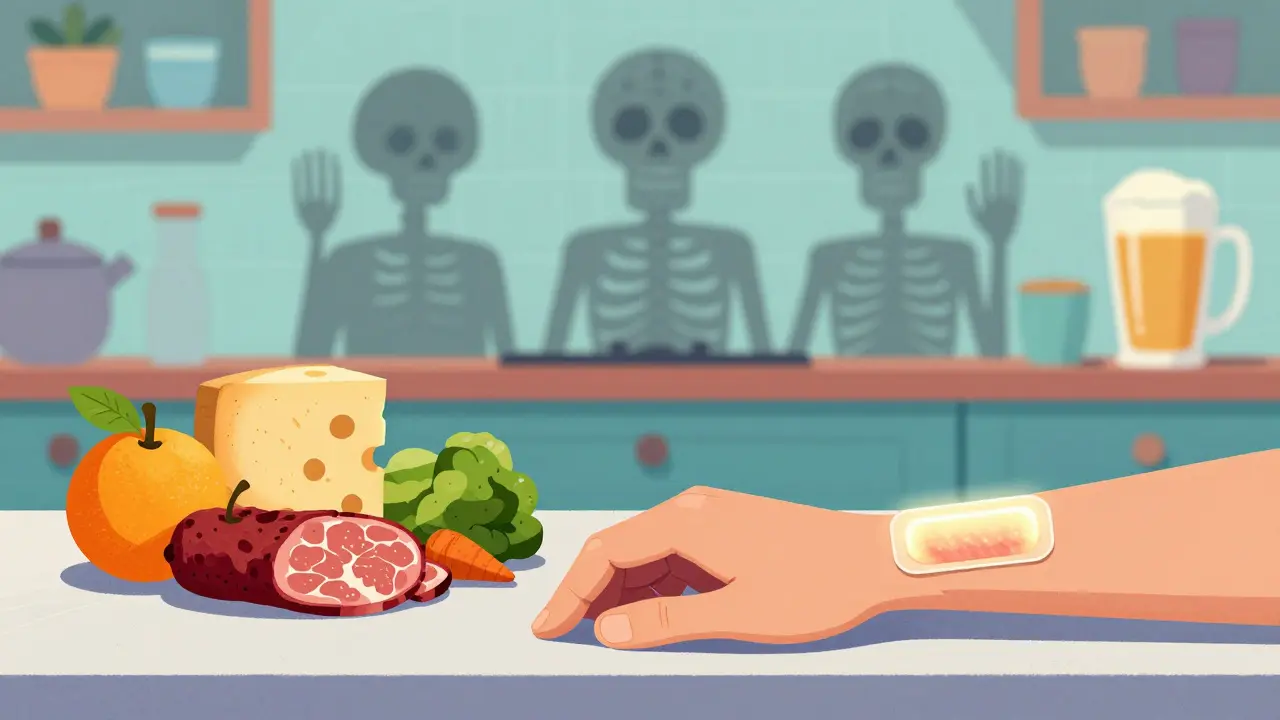
The Food Trap: What You Can’t Eat
Most people know they can’t eat aged cheese with MAOIs. But what counts as “aged”? And what else is hiding in your kitchen?
- Aged cheeses - Cheddar, parmesan, blue cheese, gouda aged over 6 months. Just one ounce can contain 15mg of tyramine-the threshold for triggering a crisis is as low as 10mg.
- Fermented soy - Soy sauce, miso, tempeh. A single tablespoon of soy sauce can have up to 30mg of tyramine.
- Cured and smoked meats - Pepperoni, salami, pastrami, hot dogs. These contain tyramine from the curing process.
- Draft and tap beer - Bottled beer is usually safe. But draft beer, especially unpasteurized, can have 8-20mg of tyramine per 12oz. Wine like Chianti has about 8mg per 5oz glass.
- Fermented foods - Sauerkraut, kimchi, pickled herring. Even small amounts can be risky.
There’s one exception: the selegiline patch (Emsam) at the lowest dose (6mg/24hr). Studies show it doesn’t interfere with tyramine metabolism at this level. Patients on this dose can eat normally. But if you switch to a higher dose, the restrictions return.
What’s Changed to Keep People Safe
Doctors didn’t ignore the risks. The system has been rebuilt around them.
Since 2004, electronic health records in the U.S. have hard stops that prevent doctors from prescribing an MAOI with a contraindicated drug. If you try to order fluoxetine while on phenelzine, the system blocks it. That was a direct response to 19 deaths between 1998 and 2003.
Psychiatrists now routinely give patients wallet cards listing every dangerous drug and supplement. A 2020 survey found 78% of psychiatrists provide them. But here’s the problem: primary care doctors don’t always know. A 2021 study showed 34% of family physicians didn’t realize dextromethorphan was off-limits.
The FDA requires warning labels on all dextromethorphan products: “Do not use if you’re taking an MAOI.” But a 2020 GAO report found 12% of products still didn’t have it.
Who Still Gets Prescribed MAOIs Today?
Less than 1% of all antidepressant prescriptions in the U.S. are for MAOIs. That number has stayed steady since 2015. Most are prescribed by psychiatrists-92% of them. Only 8% come from primary care doctors. Why? Because managing MAOIs isn’t simple. It requires detailed patient education, strict follow-up, and awareness of every medication the patient takes.
The transdermal selegiline patch now makes up 68% of all MAOI prescriptions. It’s preferred because it avoids the gut, where tyramine is normally broken down. That’s why the lowest dose doesn’t require dietary restrictions. It’s safer. But it’s still not risk-free.
What You Should Do If You’re on an MAOI
If you’re taking one, here’s your checklist:
- Carry a wallet card with every contraindicated drug and supplement listed.
- Never take OTC meds without checking with your psychiatrist or pharmacist. Even “harmless” cold pills can be deadly.
- Know your food risks. If it’s aged, fermented, or cured, assume it’s dangerous unless confirmed otherwise.
- Never stop or switch antidepressants on your own. The 14-day (or 5-week) washout period is non-negotiable.
- Wear a medical alert bracelet. In an emergency, paramedics need to know you’re on an MAOI.
If you feel sudden headache, chest pain, rapid heartbeat, high fever, confusion, or muscle stiffness-call 911. These aren’t side effects. They’re signs of a medical emergency.
Is There a Safer Future?
There’s a drug called moclobemide-a reversible MAOI used in Europe and Canada. It doesn’t carry the same food or drug interaction risks. But it was never approved in the U.S. because its antidepressant effects were seen as too mild in clinical trials. Meanwhile, the older, riskier MAOIs remain on the market.
There’s no magic bullet. MAOIs work when nothing else does. But they demand respect. A single mistake can be fatal. That’s why they’re not for everyone. But for those who need them, knowing the risks isn’t just smart-it’s the only way to stay alive.
Can I take ibuprofen with MAO inhibitors?
Yes, ibuprofen and other NSAIDs like naproxen are generally safe with MAOIs. They don’t affect serotonin or norepinephrine levels. But always check with your doctor, especially if you have high blood pressure or kidney issues, since MAOIs can already raise blood pressure.
What happens if I accidentally take a contraindicated drug?
If you take something like dextromethorphan, tramadol, or a decongestant while on an MAOI, symptoms can appear within 30 minutes to 2 hours. Watch for severe headache, chest pain, fast heartbeat, high fever, confusion, or muscle rigidity. These are signs of hypertensive crisis or serotonin syndrome. Call 911 immediately. Don’t wait. Do not try to treat it yourself.
Are all antidepressants dangerous with MAOIs?
No, but most are. SSRIs, SNRIs, tricyclics, and even some atypical antidepressants like bupropion can be dangerous. The only antidepressants considered relatively safe are those that don’t affect serotonin, like bupropion-but even then, caution is needed. Never assume safety. Always consult your prescriber before starting or stopping any medication.
Can I drink alcohol while on MAO inhibitors?
Avoid alcohol entirely. It can increase blood pressure and interact unpredictably with MAOIs. Red wine, in particular, contains tyramine and can trigger a hypertensive crisis. Even small amounts of beer or spirits carry risk. The safest approach is complete abstinence.
Is it safe to use an MAOI during pregnancy?
There’s limited data. MAOIs are not typically recommended during pregnancy due to unknown fetal risks. If you’re pregnant or planning to be, talk to your psychiatrist. Stopping abruptly can be dangerous too. A careful, individualized plan is essential.









man i had no idea dextromethorphan could be this dangerous with MAOIs. i’ve been popping cough syrup like candy during flu season. time to throw out my shelf of Robitussin.
if you're on an MAOI, just assume every OTC med is a landmine. always check with your pharmacist-they know the drug interactions better than most docs.
the selegiline patch at 6mg/24hr is the only MAOI i’d ever consider prescribing now. it bypasses gut metabolism, so tyramine doesn’t get absorbed in dangerous amounts. game-changer for compliance and safety.
in south africa, we call this ‘pharmaco-ignorance’. people think ‘natural’ = safe, so they load up on St. John’s Wort and ginseng like it’s cereal. then they end up in the ER with a 41°C fever and no idea why. education isn’t optional-it’s survival.
the FDA’s hard stops in EHRs saved lives, but they’re only as good as the data feeding them. i’ve seen systems flag tramadol but miss linezolid because it’s coded as an ‘antibiotic’ not an MAOI. we need better ontology standards across clinical databases.
AMERICA NEEDS TO STOP LETTING PEOPLE BUY DEXTROMETHORPHAN LIKE IT’S CANDY 🇺🇸🚫💊
they say MAOIs are ‘old-school’ like rotary phones-but guess what? rotary phones still work when the internet crashes. same with MAOIs. when SSRIs fail, these are the last bullets in the chamber. stop acting like they’re dinosaurs-they’re tactical nukes with instructions.
if you’re on an MAOI and you’re scared, you’re doing it right. this isn’t about being paranoid-it’s about being prepared. carry that wallet card. wear the bracelet. tell your barista. your life depends on people knowing what’s in your system.
the real tragedy isn’t the deaths-it’s the systemic cowardice. we let a drug with 12% mortality risk stay on the market while we ban safer alternatives like moclobemide because it’s ‘too mild.’ this isn’t medicine-it’s a morality play where patients are the sacrificial lambs. we glorify risk when it’s profitable, and call it ‘progress.’
the 14-day washout period is non-negotiable. i’ve seen patients switch from sertraline to phenelzine in 7 days because they ‘felt better.’ they didn’t. they ended up in ICU. this isn’t a suggestion-it’s a physiological law.
in india, many people take st. john’s wort with ayurvedic meds and don’t even know they’re on an MAOI. doctors here rarely warn them. this post is a wake-up call. i’m printing it out for my uncle-he’s on phenelzine and drinks soy sauce with rice daily.
so let me get this straight-we have a drug that can kill you if you eat cheese, drink beer, or take a cough drop… but we still let people buy it over the counter? brilliant. just add a skull and crossbones and call it ‘MAOI: The Game of Death.’
they don’t want you to know this… but the FDA and pharma companies are hiding moclobemide because it’s cheaper and safer. they make more money off the dangerous ones. they want you dependent. they want you scared. they want you buying pills forever. wake up.
the true paradox of MAOIs is this: they’re the most dangerous antidepressants, yet also the most effective for treatment-resistant cases. in philosophy, we call this the ‘necessity of risk’-some truths demand sacrifice. the real question isn’t whether they’re safe, but whether we’re willing to treat them with the reverence they deserve.