Drug Interactions: How Food, Supplements, and Medications Can Clash

Imagine taking your blood pressure pill with a glass of grapefruit juice, or popping a St. John’s wort supplement while on antidepressants. Sounds harmless, right? But these everyday choices can turn dangerous-fast. Drug interactions aren’t just rare side effects. They’re a silent, widespread threat that lands tens of thousands in hospitals every year. And most people have no idea they’re at risk.
Why Your Breakfast Could Be Sabotaging Your Medication
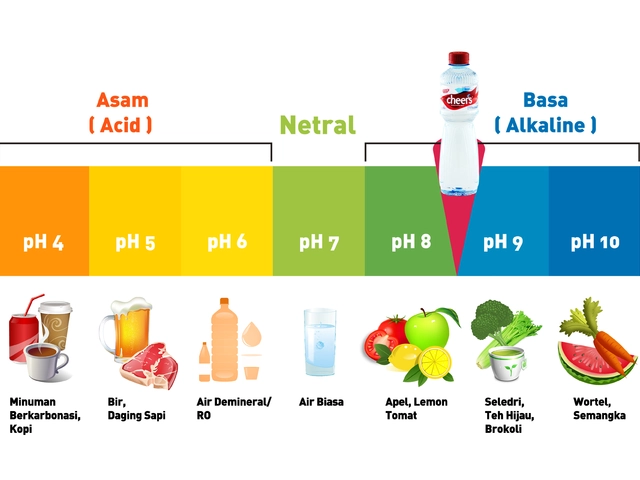
Grapefruit juice isn’t just a tangy start to your day. It’s a chemical wildcard that can wreck how your body handles certain drugs. The problem? Furanocoumarins in grapefruit block an enzyme in your gut called CYP3A4. This enzyme normally breaks down medications so they don’t build up to toxic levels. When it’s shut down, drugs like simvastatin (a cholesterol-lowering statin) can spike in your bloodstream by up to 15 times. That’s not a typo. A 2004 study in the Canadian Medical Association Journal found this spike pushes the risk of rhabdomyolysis-a condition where muscle tissue breaks down and can cause kidney failure-from 0.15 cases per 100,000 people to nearly 1.6 per 100,000. One glass of juice. One dangerous change. It’s not just grapefruit. Pomegranate juice, Seville oranges, and even some types of pomelo do the same thing. And if you’re on a statin, a calcium channel blocker, or certain immunosuppressants like cyclosporine, you’re in the danger zone. The fix? Simple: swap grapefruit for orange or apple juice. But only if your doctor says it’s safe.Leafy Greens and Blood Thinners: A Hidden Battle
If you’re on warfarin (Coumadin), your salad might be working against you. Vitamin K, found in spinach, kale, broccoli, and Brussels sprouts, directly counteracts warfarin’s ability to thin your blood. It doesn’t matter if you eat one big bowl or a handful every day. What matters is consistency. A 2018 study in the Journal of Thrombosis and Haemostasis showed that eating just 150 grams of cooked spinach-about a cup and a half-can drop warfarin’s effect by 30-40% within 24 hours. That means your blood clots faster. You could develop a clot in your leg, lung, or brain. The FDA has documented over 28 cases of dangerous bleeding from cranberry juice and warfarin, with INR levels (a measure of blood clotting) spiking above 8.0. Normal range? 2.0 to 3.0. The solution isn’t to stop eating greens. It’s to eat the same amount every day. The National Academy of Medicine recommends 90 mcg of vitamin K daily for women and 120 mcg for men. Stick to that. Don’t go from spinach salad every day to no greens for a week. Your blood thinner needs predictability.Supplements: The Wild West of Medication Safety
Dietary supplements aren’t regulated like drugs. That means no rigorous testing, no mandatory warnings, and no guarantee they even contain what’s on the label. Yet 40% of American adults take them-and most never tell their doctor. St. John’s wort is the most dangerous supplement you’ve probably never heard of. It triggers liver enzymes that break down over half of all prescription drugs. People on birth control have gotten pregnant after taking it. Those on antidepressants have slipped into serotonin syndrome-fever, shaking, rigid muscles, and sometimes death. A 2000 study in Clinical Pharmacology & Therapeutics showed it cuts cyclosporine levels by 50-70%. That’s enough to make a transplant patient reject their new organ. Ginkgo biloba? It thins the blood. If you’re on aspirin, warfarin, or clopidogrel, you’re increasing your risk of brain bleeds. A 2001 study in Annals of Pharmacotherapy tracked 32 cases where garlic supplements caused dangerous bleeding when mixed with blood thinners. Red yeast rice? It’s basically natural statins. Take it with a prescription statin like atorvastatin? Your risk of muscle damage jumps 2.3 times, according to a 2017 study in the Journal of the American College of Cardiology. And here’s the kicker: only 29% of supplement labels carry any interaction warning. The FDA says 23% of serious supplement-related hospital visits between 2013 and 2019 were from interactions. You’re gambling with your health every time you open a bottle without asking a professional.
What You Need to Do Right Now
This isn’t about fear. It’s about control. You don’t have to stop taking supplements. You don’t have to give up your favorite foods. But you need to know what’s in your body-and what’s in your medicine cabinet. Start with a complete list: every prescription, every over-the-counter pill, every vitamin, herb, or supplement. Write it down. Include dosages and how often you take them. Update it every time you see a doctor or pharmacist. Bring that list to every appointment. Don’t assume your doctor knows. A 2022 editorial in JAMA Internal Medicine found 70% of patients don’t mention supplements unless asked. That’s not your fault-it’s a system failure. But you can fix it. Use free tools. MedlinePlus has a drug interaction checker that covers 3,500+ medications and supplements. The LiverTox database from the NIH lists over 1,200 verified interactions with clinical evidence ratings. These aren’t guesswork-they’re science-backed.When to Call Your Doctor Immediately
Some interactions don’t wait. If you start taking something new and notice:- Sudden muscle pain or weakness (especially with statins)
- Unexplained bruising or bleeding (nosebleeds, bloody stools, heavy periods)
- Confusion, fever, rapid heartbeat, or stiff muscles (signs of serotonin syndrome)
- Swelling in your legs or trouble breathing (possible blood clot)

How Pharmacists Can Save Your Life
Pharmacists aren’t just the people who hand you pills. They’re trained interaction detectives. A 2022 report from the American Society of Health-System Pharmacists found that pharmacist-led medication reviews cut adverse drug events by 21.7%. That’s one in five fewer hospital visits. Ask your pharmacist to run a full interaction check every time you pick up a new prescription. They can spot conflicts between your statin and grapefruit, your blood thinner and ginkgo, or your antidepressant and St. John’s wort. They can also tell you if a supplement is even worth taking-many are useless or dangerous. And if your pharmacy doesn’t offer this? Ask them to start. You’re paying for their expertise. Use it.The Future Is Here-But You Still Have to Act
Technology is catching up. AI tools like IBM Watson Health can now predict new drug-supplement interactions by analyzing millions of medical notes with 87% accuracy. Electronic health records now flag high-risk combinations before a doctor even prescribes. The FDA’s Sentinel Initiative is tracking real-world data from 190 million Americans to spot patterns no lab study ever could. But none of this helps if you don’t speak up. No algorithm will know you’re taking turmeric capsules because your friend said it helps arthritis. No AI will catch that you swapped your orange juice for grapefruit because it tastes better. Your body is the final system. You’re the last line of defense.What to Remember
- Never mix supplements with prescriptions without checking first.
- Keep vitamin K intake steady if you’re on warfarin-don’t quit greens, just keep them consistent.
- Avoid grapefruit, pomegranate, and Seville oranges if you take statins, blood pressure meds, or immunosuppressants.
- Always carry a full list of everything you take-including doses and frequency.
- Ask your pharmacist to check for interactions every time you get a new prescription.
- Call your doctor immediately if you feel unusual muscle pain, bleeding, confusion, or rapid heartbeat after starting something new.
Medication safety isn’t about being perfect. It’s about being aware. One conversation with your pharmacist, one updated list, one question asked-could be the difference between staying healthy and ending up in the ER.
Can I still drink grapefruit juice if I’m not on medication?
Yes-if you’re not taking any prescription drugs, grapefruit juice is safe for most people. But if you start a new medication later, even a blood pressure pill or cholesterol drug, you’ll need to stop. The interaction doesn’t show up until you combine the two. So if you’re planning to take any new medicine, it’s smarter to avoid grapefruit altogether.
Are natural supplements safer than prescription drugs?
No. Just because something is “natural” doesn’t mean it’s safe. St. John’s wort, ginkgo, garlic, and red yeast rice are all plant-based, yet they can cause life-threatening interactions. The FDA doesn’t require supplement makers to prove safety or effectiveness before selling them. That’s the opposite of prescription drugs, which go through years of testing. Natural doesn’t mean risk-free.
I take fish oil. Is that safe with blood thinners?
Fish oil has mild blood-thinning effects. For most people taking low doses (under 3 grams per day), it’s fine. But if you’re on warfarin, clopidogrel, or aspirin, even low-dose fish oil can increase bleeding risk. Talk to your doctor before continuing. They may suggest a lower dose or switch you to a different omega-3 source. Don’t assume it’s harmless just because it’s healthy.
Can I use a drug interaction app instead of asking my doctor?
Apps like MedlinePlus or Drugs.com are great tools-but they’re not replacements for professional advice. They can miss rare interactions, outdated studies, or your unique health history. A pharmacist or doctor knows your full medication list, kidney/liver function, allergies, and other conditions. An app doesn’t. Use apps to check, but always confirm with a healthcare provider.
What if I forget to tell my doctor about my supplements?
It happens to everyone. But the longer you wait, the more risk you take. The next time you’re in for a checkup, bring your supplement bottles or a written list. Say: “I’ve been taking these, but I didn’t think they mattered.” Most doctors will appreciate the honesty and help you adjust. Don’t wait for a bad reaction to speak up.
Are there any supplements that are generally safe with most medications?
Calcium and vitamin D are usually safe in standard doses, as long as you’re not on thyroid medication like levothyroxine (they can interfere with absorption if taken together). Multivitamins without herbal extracts are often low-risk. But “generally safe” doesn’t mean “always safe.” Always check. Even something as simple as magnesium can lower blood pressure too much if you’re already on a beta-blocker. Never assume.








The CYP3A4 enzyme inhibition by grapefruit isn't just about statins-it's a pharmacokinetic wildcard that affects nearly 50% of oral medications. The furanocoumarins irreversibly inhibit intestinal CYP3A4, and since the enzyme doesn't regenerate quickly, even a single serving can have a 72-hour window of risk. Most patients don't realize this isn't a dose-dependent issue-it's a mechanism-based inactivation. The clinical takeaway? It's not about quantity, it's about presence. Even occasional consumption can destabilize therapeutic drug levels, especially with narrow therapeutic index agents like cyclosporine or tacrolimus. This isn't scare tactics-it's biochemistry in motion.
And let's not forget the genetic variability: poor metabolizers with CYP3A5*3 polymorphisms are even more vulnerable. We're not talking about anecdotal risk. We're talking about population-level pharmacovigilance data that's been replicated across multiple continents.
Pharmacists should be screening for grapefruit juice intake like they screen for smoking or alcohol use. It's that critical.
Also, pomegranate juice? Same mechanism. Seville oranges? Same. Even some pomelos. The label doesn't always say it. You have to know the botanicals.
Bottom line: if you're on anything metabolized by CYP3A4, treat grapefruit like a contraindication, not a suggestion.
It is, regrettably, a profound failure of public health education that individuals continue to conflate "natural" with "safe." The assumption that botanical substances are inherently benign reflects a dangerous romanticization of pre-scientific medicine. St. John’s wort, for instance, is not a "herbal remedy"-it is a potent cytochrome P450 inducer with documented, life-threatening interactions. The fact that it is sold without a prescription does not imply regulatory approval; it implies regulatory neglect. The FDA’s inability to mandate pre-market safety testing for dietary supplements is a legislative abdication, not a testament to consumer freedom. One must ask: if a substance can alter the pharmacokinetics of life-sustaining medications, why is it not classified as a drug? The answer lies in lobbying, not science.
It is not enough to "ask your doctor." One must demand a complete pharmacological review-not a perfunctory nod at the end of a 10-minute visit. Your pharmacist, trained in pharmacokinetics and drug metabolism, is your most underutilized safeguard. Treat them as such.
Okay but have you ever thought about how Big Pharma is totally hiding this? I mean, grapefruit juice doesn't have a patent, right? So why would they want you to know that a $2 fruit can mess up their $200-a-pill statin? And don't get me started on how the FDA is basically in bed with supplement companies-look at the loophole in DSHEA from 1994, it's like they wrote it to let companies sell snake oil and call it "wellness."
And St. John’s wort? That's been used for centuries by ancient Greeks and now suddenly it's "dangerous" because a lab study says so? I bet they're just scared people will stop buying antidepressants and start using sunshine and herbal tea instead. I mean, why else would they not fund proper studies on natural alternatives? They don't want you to be healthy-they want you dependent.
Also, I read on a forum that grapefruit juice actually helps with detoxing your liver. So maybe the enzyme inhibition is a good thing? Maybe your body is just trying to cleanse itself? I don't know. But I'm not taking anything from a pharmacy anymore. I'm going full ancestral. No pills. Just lemon water, cold showers, and turmeric shots. My cholesterol dropped 30 points in 3 weeks. Coincidence? I think not.
And why do they say "consult your doctor" like that's the end-all? Your doctor works for the system. They're paid by insurance companies. They don't want you to know the truth. The truth is: you're being sold fear to keep you buying pills. Break free. Research yourself. Question everything.
P.S. I started taking garlic supplements with my blood thinner and I feel more alive than ever. My blood is "thinner"-like, literally thinner. I think it's a sign I'm on the right path.
P.P.S. If you're not taking supplements, you're probably being poisoned by the system. Just saying.
This is one of those posts that should be required reading before you even get your first prescription. I didn’t know half this stuff until my grandma ended up in the hospital after mixing warfarin with a new ginkgo supplement she got from the health food store. She thought "natural" meant "can’t hurt."
I now keep a printed list of everything I take-prescriptions, OTC, vitamins, even the fish oil I take for my knees-and I bring it to every appointment. My pharmacist actually remembers me now. That’s huge.
Also, I switched from grapefruit juice to orange juice years ago after my cardiologist told me. I didn’t even like orange juice before-but now I don’t miss it. Small change, big difference.
Don’t overcomplicate it. Just know what’s in your body. Talk to your pharmacist. Don’t assume. Ask. Even if it feels awkward. It’s worth it.
Let’s be real-most people treat their meds like candy. 🍬 You pop a statin, drink grapefruit juice, take St. John’s wort because "it’s natural," then wonder why you’re dizzy and your muscles feel like jelly. 🤯
And don’t even get me started on the supplement industry. It’s a $50 billion scam where companies slap "clinically proven" on a bottle of powdered roots and charge $40. The FDA doesn’t regulate it? That’s not freedom-that’s negligence. You wouldn’t eat random mushrooms from the woods and call it medicine. Why do you think a capsule labeled "Ginkgo Biloba 120mg" is any different?
And yes, I know you’re going to say "but my yoga instructor said it helps my anxiety!" Cool. So did heroin. That doesn’t make it safe. 🙄
Bottom line: if you’re taking more than three supplements, you’re probably just wasting money and risking your life. Stop trying to biohack yourself into perfection. Just take your meds, eat your greens consistently, and talk to a real doctor. Not a wellness influencer.
This is the kind of information that changes lives-and it’s not being shared enough. I’ve been teaching a senior wellness class for five years now, and every single session, someone walks away saying, "I had no idea."
Here’s what I tell them: You don’t need to be perfect. You just need to be aware. One conversation. One list. One question. That’s all it takes.
Bring your bottles to your pharmacist. Write down your supplements. Say, "I’m taking this, but I’m not sure if it’s okay." They won’t judge you. They’ll thank you.
And if you’re on warfarin-yes, eat your spinach. But eat the same amount every week. Consistency is your superpower.
Knowledge isn’t power. Applied knowledge is. Start today. You’ve got this.
Life is a balance. Not control. Not fear. Just awareness.
They sell pills. They sell juice. They sell hope.
Who profits?
Pharmacists are the unsung heroes of medication safety. A 2022 ASHP report showed pharmacist-led interventions reduce adverse drug events by over 20 percent. Yet most patients never ask. Why? Because we’ve been conditioned to see doctors as the sole authority. But pharmacists are the ones who actually read the interactions, check the databases, and know the nuances. They are the final checkpoint before the medication reaches you. Use them. Respect them. Ask them to run a full interaction screen every time you pick up a new script. It’s free. It’s professional. It’s life-saving. Do it.
Wait-so you’re telling me that I can’t have my morning grapefruit juice if I’m on a statin? But I’ve been doing it for 15 years and I feel fine! And now you want me to stop? And pay more for orange juice? And carry a list? And ask my pharmacist? And stop taking my "miracle" turmeric capsules? This is ridiculous. I’ve never been hospitalized. I’m 72. I’ve survived worse. This is just fear-mongering by the medical-industrial complex. You want me to live in a bubble? No thanks. I’ll take my juice, my supplements, and my peace of mind. And if I die? At least I died on my terms. Not someone else’s protocol.
Also, I read that vitamin K in greens is good for bones-so maybe warfarin is the real problem? Maybe they should just stop prescribing it? Or maybe I should switch to one of those new blood thinners? But those are expensive. And I don’t trust them. They’re too new. So I’ll stick with my warfarin-and my spinach. And my grapefruit. And my St. John’s wort. Because I’m not a lab rat. I’m a human being.
And if you’re telling me I can’t have what I like because some study says so? Then you’re not helping. You’re controlling.