Insurance and Medication Changes: How to Navigate Formularies Safely

Medication Cost Calculator
Check your prescription costs and understand how formulary changes affect your out-of-pocket expenses. Input your medications to see estimated costs by tier.
Find Your Medication Costs
Results
Enter your medication to see estimated costs and recommendations.
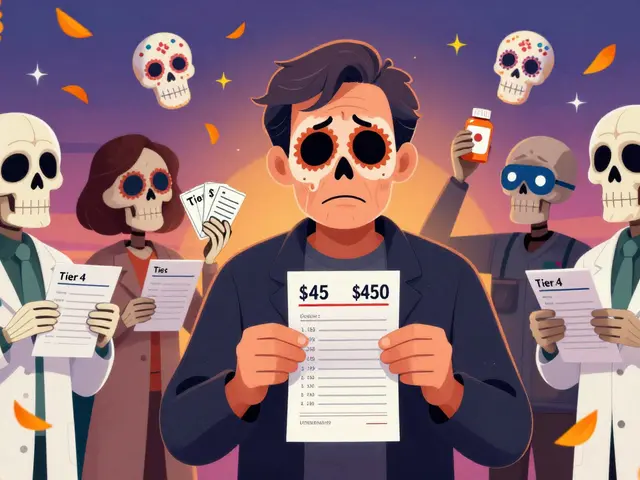
When your insurance plan changes the list of drugs it covers, it’s not just a paperwork update-it can mean your monthly bill jumps from $45 to $450 overnight. This isn’t rare. In 2023, over 12% of Medicare beneficiaries had at least one of their medications removed from their plan’s formulary. For people managing chronic conditions like diabetes, heart disease, or depression, that kind of shift can derail treatment, cause delays, or even lead to worse health outcomes.
What Exactly Is a Formulary?
A formulary is the official list of prescription drugs your insurance plan will pay for. It’s not random. Every drug on the list has been reviewed by a team of doctors and pharmacists who decide which medications offer the best balance of safety, effectiveness, and cost. Most plans use a tier system to show how much you’ll pay for each drug.- Tier 1: Generic drugs. Usually $0-$10 per prescription.
- Tier 2: Preferred brand-name drugs. Around $25-$50.
- Tier 3: Non-preferred brand-name drugs. $50-$100.
- Tier 4 or 5: Specialty drugs. Often $100+ or a percentage of the total cost.
Why Do Formularies Change?
Formularies aren’t set in stone. They’re updated every year, usually on January 1. But changes can also happen mid-year. About 23% of plans make changes outside the annual cycle. Why? Because new generic versions come out, drugs get recalled, or insurers negotiate better prices with drug makers. Medicare Part D plans have to cover all drugs in six protected classes: antidepressants, antipsychotics, immunosuppressants, HIV/AIDS drugs, anticonvulsants, and cancer treatments. Commercial plans don’t have that rule. That means if you’re on a commercial plan, your insurer could drop a critical medication with fewer legal restrictions. In 2023, the Inflation Reduction Act forced Medicare Part D plans to remove cost-sharing for insulin-so nearly all plans now cover insulin at $35 a month. That’s a huge win. But for other drugs, especially specialty ones, insurers are tightening control. About 47% of commercial plans now require prior authorization for specialty drugs, compared to just 32% of Medicare plans.How to Check Your Formulary Before It’s Too Late
Most people don’t check their formulary until their prescription is denied at the pharmacy. Don’t wait. Here’s how to stay ahead:- Find your plan name. It’s on your insurance card. Write it down.
- Go to your insurer’s website. Look for "Drug List," "Formulary," or "Prescription Coverage." It’s often buried under "Plan Materials" or "Member Resources."
- Search for every medication you take. Type in the exact name, including brand and generic versions.
- Note the tier and any restrictions. Is it on the list? Is there a prior authorization or step therapy requirement?
- Check the date. Make sure you’re looking at the current year’s formulary. Many sites still show last year’s list.
What to Do If Your Drug Gets Removed
If your medication is taken off the formulary, you’re not out of options. Most plans allow you to request an exception. Here’s how to do it right:- Ask your doctor to file a prior authorization or exception request. They need to explain why the alternative drugs won’t work for you.
- Use proven reasons. The most successful requests are based on:
- Previous treatment failure (47% of approved cases)
- Adverse reaction to alternatives (32%)
- Don’t wait. CMS data shows 78% of doctor-submitted exceptions are approved within 72 hours. But if you wait too long, you might run out of medication.

When to Switch Plans
If your medications keep getting bumped to higher tiers or are removed entirely, it might be time to switch insurance plans. For Medicare beneficiaries, the Annual Enrollment Period runs from October 15 to December 7 each year. That’s your chance to compare plans and pick one that covers your drugs at the lowest cost. Use the Medicare Plan Finder tool. It lets you enter your medications and see which plans cover them and how much you’ll pay. Don’t rely on the default recommendation-it often picks the cheapest plan overall, not the one that’s cheapest for you. For commercial plans, check your options during your employer’s open enrollment period. Some employers let you switch plans mid-year if you have a qualifying life event-like a new diagnosis or a change in medication.Big Trends Shaping Formularies in 2025
The rules are changing fast. Starting in 2025, Medicare Part D will cap out-of-pocket drug costs at $2,000 per year. That’s going to reduce the pressure on insurers to restrict access to expensive drugs. But it’s also going to mean more drugs are added to higher tiers, because insurers will want to keep costs low elsewhere. Pharmacy benefit managers (PBMs)-companies like CVS Caremark and Express Scripts-control about 87% of commercial formularies. They’re under fire for steering patients toward drugs that give them the biggest rebate, not necessarily the best ones. In June 2023, the FTC sued major PBMs for anti-competitive behavior. Newer trends include:- AI-driven formularies: 37% of PBMs now use AI to predict which drugs will be most cost-effective based on real-world usage data.
- Specialty tiers: More drugs are being pushed into high-cost tiers. By 2026, over half of all specialty drugs will be in Tier 5.
- Real-world evidence: Insurers are starting to use data from patient outcomes-not just clinical trials-to decide which drugs stay on the list.
How to Protect Yourself
Here’s a simple checklist to avoid surprises:- Review your formulary every October. Even if you’re not switching plans, check for changes.
- Set calendar reminders for your medication refill dates. Don’t let them expire right after a formulary update.
- Ask your pharmacist. They see formulary changes daily. They can tell you if your drug is at risk.
- Keep a list of all your medications, doses, and why you take them. This helps your doctor make a stronger case if you need an exception.
- Know your rights. Insurers must notify you in writing if they’re removing a drug you take. For Medicare, that notice must come 60 days in advance. For commercial plans, it’s 30 days.

What Happens If You Skip This Step?
A 2023 study by the National Council on Aging found that a 72-year-old cancer patient went 21 days without her medication after it was removed from the formulary. No warning. No notice. She had to go to the ER. Another patient skipped checking their formulary and found out their antidepressant was no longer covered. They tried switching to a cheaper one-but it made them feel worse. They didn’t tell their doctor for weeks because they didn’t want to be a "burden." By then, their depression had worsened. Formularies are meant to save money. But when they’re poorly managed, they cost more-in health, stress, and time.Frequently Asked Questions
What if my insurance drops my medication but doesn’t offer a good alternative?
You can request an exception based on medical necessity. Your doctor must document why other drugs won’t work-for example, if you’ve had side effects or the alternatives failed in the past. If your request is denied, you can appeal. Many states have patient advocacy offices that can help you navigate this process.
Can I get my medication covered if it’s not on the formulary at all?
Yes, but it’s harder. You’ll need a prior authorization request from your doctor that proves the drug is medically necessary and that no formulary alternatives are suitable. Some plans also have a "non-formulary drug request" process, but approval rates are lower-especially for non-specialty drugs.
Why do some drugs have step therapy requirements?
Step therapy means you must try cheaper, approved drugs first before the insurer will cover the one your doctor prescribed. It’s meant to reduce unnecessary spending on expensive drugs when cheaper ones work just as well. For chronic conditions like rheumatoid arthritis or multiple sclerosis, studies show step therapy reduces high-cost use by 18% without hurting outcomes-if it’s applied fairly.
How do I know if a drug is generic or brand-name on the formulary?
Generic drugs are listed by their chemical name (like "metformin"), while brand names include the trademark (like "Glucophage"). Most formularies list both. If you’re unsure, ask your pharmacist or search the drug name on Drugs.com-it’ll tell you if it’s generic or brand.
Are there any drugs that insurance must cover no matter what?
Yes, but only under Medicare Part D. Plans must cover all drugs in six protected classes: antidepressants, antipsychotics, immunosuppressants, HIV/AIDS drugs, anticonvulsants, and cancer treatments. Commercial plans have no such requirement. Always check your plan’s rules.
What should I do if I can’t afford my medication after a formulary change?
Contact your pharmacy. Many drug manufacturers offer patient assistance programs that give free or discounted medications to people who qualify. You can also check with nonprofit groups like NeedyMeds or the Patient Access Network Foundation. Some pharmacies, like CVS and Walgreens, have discount programs for common medications.






Just checked my formulary after reading this-turns out my diabetes med got moved to Tier 4. I called my pharmacist and they helped me file a prior auth same day. Took 36 hours. No drama. Don’t wait until you’re out of pills.
Let’s be real-this whole system is a rigged game designed by PBMs who get kickbacks from Big Pharma. Insurers don’t care about your health, they care about their rebate percentages. That’s why your $35 insulin is covered but your $800 antidepressant isn’t. It’s not medical necessity-it’s corporate greed wrapped in a formulary. And don’t get me started on how they use AI to predict which drugs you’ll stop taking so they can drop them faster. This isn’t healthcare. It’s a financial instrument disguised as a safety net.
Thank you for this. I’ve been through the nightmare of having my heart med kicked off formulary. Took me six weeks, three doctors’ letters, and a lot of crying in the pharmacy parking lot. But I did it. You can too. Don’t give up. Keep pushing. Your life matters more than their paperwork.
As someone who works in patient advocacy, I see this every week. The biggest mistake people make? Waiting until the pharmacy says ‘no’ before acting. Start checking your formulary in September. Set a calendar reminder. Print it. Keep it in your wallet. And if your doctor won’t fight for you, find another one. Your meds aren’t optional-they’re your lifeline.
The author’s tone is excessively alarmist and lacks scholarly rigor. The data cited is cherry-picked from Consumer Reports and CMS, neither of which are peer-reviewed sources. Moreover, the assertion that commercial plans lack protections for protected classes is misleading-ERISA plans are governed by federal statutes that impose fiduciary duties. The article reads like a lobbying pamphlet disguised as public service journalism.
People who don’t check their formulary deserve what they get. I’ve been on the same meds for 12 years. I check every October. I call my pharmacist every time there’s a change. I keep a binder. If you can’t be responsible for your own health, don’t blame the system. You’re the one who didn’t read the fine print.
Let me break this down for you. If your drug gets dropped, call your doctor’s office and say ‘I need a prior auth for [drug name] because I’ve tried alternatives and had adverse reactions.’ That’s it. No drama. No waiting. Most are approved in under 72 hours. The system works if you know how to use it. And if your doctor won’t help, find one who will. Your life is worth fighting for. Don’t let bureaucracy win.
Hey, I’m not a doctor but I’ve been on 14 different meds since 2018 and I’ve got a spreadsheet. You wanna know which PBMs are the worst? CVS Caremark. They’re the ones pushing step therapy on everything. I called them last month and they said ‘we’re not required to tell you why we removed it.’ That’s illegal. I filed a complaint with the state. You should too. Don’t just accept it. Fight back.
My mom’s on Medicare. She didn’t check her formulary. Got dropped from her antidepressant. Took her three weeks to get it back. She cried every night. Don’t be her. Check your list. Now.
Are you SERIOUS?! I just found out my insulin is now covered but my anxiety med is GONE?! I’ve been on it for 8 years! This is a conspiracy! The government is letting Big Pharma control our brains! I’m not taking anything else! I’m going to the pharmacy with a sign that says ‘MY MEDS ARE NOT A COMMODITY’! They’re trying to turn us into zombies! I’ve seen the documents-PBMs are working with the CIA! I’m not crazy, I’m just awake!
Wait, so you’re telling me the insurance company can just yank your meds and you’re supposed to sit there and wait? That’s not right. My cousin’s cousin’s neighbor’s dog got sick because they couldn’t get their meds. It’s all rigged. I think the government is doing this on purpose so people die and they save money. I saw a video on TikTok about it. They’re putting tracking chips in the pills now. Don’t take anything unless you know the batch number.
They’re playing us. PBMs are the real villains. They’re not even real companies-they’re ghost entities owned by hedge funds that don’t even have offices. They pull the strings behind the scenes. Your doctor doesn’t control your meds-some suit in a cubicle in New Jersey does. And they don’t care if you die. They care if the rebate check clears. This isn’t healthcare. It’s a blood sport. And you’re the prey.