Systemic Lupus Erythematosus: Symptoms, Flares, and How to Manage It

Systemic lupus erythematosus, or SLE, isn’t just one disease-it’s a body-wide rebellion. Your immune system, which should protect you, starts attacking your own skin, joints, kidneys, heart, and even your brain. It doesn’t happen overnight. For many, it starts with fatigue so deep it doesn’t go away after sleep, or a rash that shows up after a day in the sun. What begins as mild discomfort can turn into life-threatening organ damage if left unchecked.
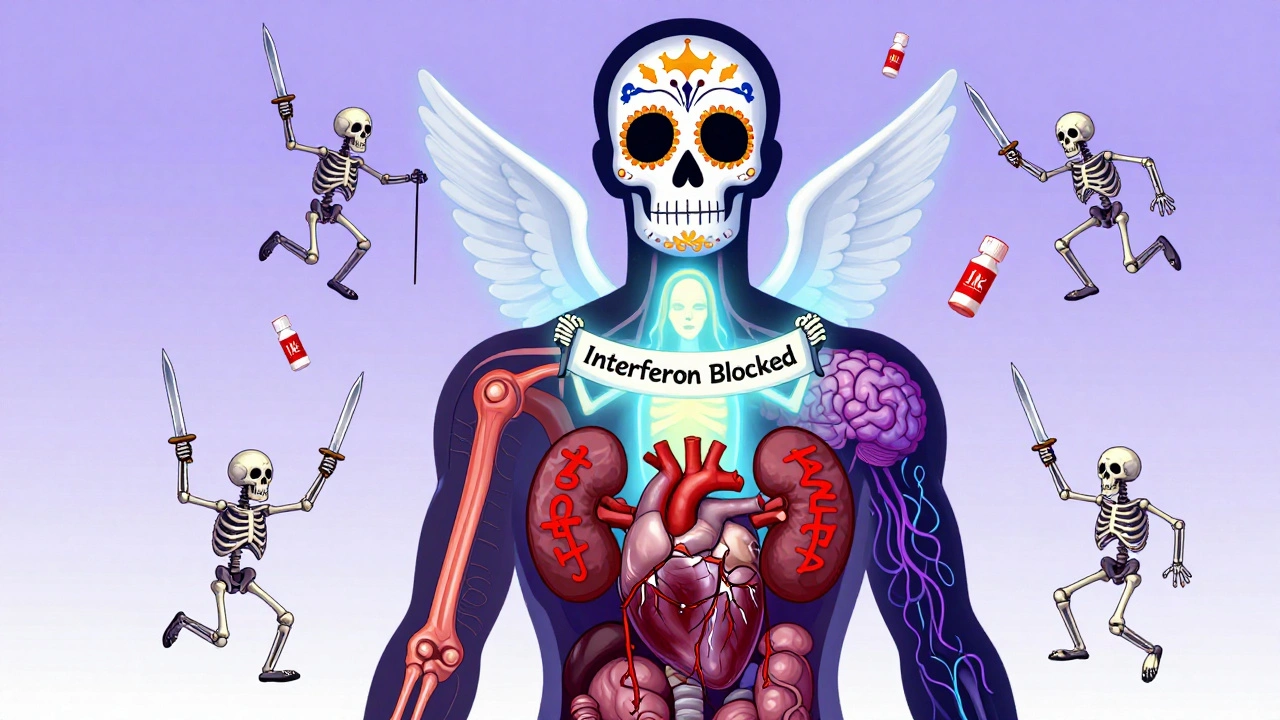
What Lupus Actually Does to Your Body
Lupus doesn’t pick one target. It hits multiple systems at once. About 95% of people with SLE experience joint pain or swelling at some point. Fatigue hits 9 out of 10. These aren’t normal tiredness or a bad day-they’re constant, crushing, and don’t improve with rest.
The classic "butterfly rash" across the cheeks and nose is what most people picture. But not everyone gets it. More common are skin changes like discoid lupus: thick, scaly, coin-shaped patches that scar and leave permanent hair loss if they appear on the scalp. Then there’s subacute cutaneous lupus-a red, scaly rash that spreads across the arms, shoulders, and neck, triggered almost always by UV light. Up to 90% of people with this form test positive for Anti-Ro (SSA) antibodies.
Beneath the skin, lupus can quietly wreck internal organs. Half of all patients develop lupus nephritis, where the kidneys become inflamed. Without treatment, this leads to kidney failure. Around 30% face heart or lung problems-pericarditis (inflammation around the heart), or pleuritis (lung lining swelling)-causing chest pain that worsens with breathing. Neuropsychiatric symptoms like memory loss, seizures, or depression affect up to 23%. Blood counts often drop: anemia, low white cells, or low platelets aren’t rare-they’re expected.
What Triggers a Lupus Flare?
A flare isn’t random. It’s your body’s alarm system going off. The triggers are known, even if they’re not always avoidable.
Sunlight is the #1 environmental trigger. UV rays don’t just cause a rash-they can kickstart a full-body flare. That’s why daily SPF 50+ sunscreen and wide-brimmed hats aren’t optional-they’re medical necessities.
Some medications can mimic or worsen lupus. Hydralazine (for high blood pressure), procainamide (for heart rhythm), and even some TNF inhibitors used for arthritis can cause drug-induced lupus. Hydrochlorothiazide, a common diuretic, is strongly linked to subacute cutaneous lupus. If you’re on any of these and develop new rashes or joint pain, talk to your doctor.
Pregnancy is another major trigger. About 50% of women with SLE experience flares during or right after pregnancy. Risks include preterm birth, preeclampsia, and miscarriage. That’s why planning is critical-getting lupus under control before conceiving cuts those risks dramatically.
Stress, infections, and lack of sleep also play roles. While we can’t measure stress’s exact impact, patients consistently report flares after major life events-job loss, divorce, the death of a loved one. It’s not "all in your head." It’s biology.
How Lupus Is Diagnosed
There’s no single test for lupus. Diagnosis is a puzzle. The 2019 classification criteria from the American College of Rheumatology and European League Against Rheumatism require a positive antinuclear antibody (ANA) test as the entry point. But here’s the catch: 95% of people with lupus have ANA-but so do 15% of healthy people. That’s why specificity matters.
More telling are anti-dsDNA and anti-Smith antibodies. Anti-dsDNA shows up in 60-70% of SLE cases and often rises during flares. Anti-Smith is rarer (20-30%) but nearly unique to lupus. Antiphospholipid antibodies are also tested-they increase the risk of blood clots and miscarriages.
Doctors combine these with clinical signs: rashes, joint pain, kidney protein in urine, low blood counts, or inflammation markers. A score of 10 or higher (out of 17) confirms SLE. Many patients wait years for diagnosis because symptoms come and go. That’s why tracking symptoms in a journal helps.

Current Treatment Strategies
Treatment isn’t one-size-fits-all. It’s layered, based on what’s damaged and how badly.
Hydroxychloroquine (Plaquenil) is the foundation for nearly every patient. It reduces flares by 50%, lowers the risk of blood clots, and improves survival. The goal is 5 mg per kg of body weight daily-no more, no less. Too little won’t help. Too much can damage the eyes, so annual eye exams are mandatory.
For skin rashes, topical steroids and antimalarials work well. For joint pain, NSAIDs like ibuprofen may help short-term. But for anything beyond mild symptoms, you need stronger tools.
When organs are involved, corticosteroids like prednisone become necessary. For severe flares-like kidney or brain involvement-doctors use pulse methylprednisolone: 500-1000 mg IV for three days. It’s powerful, but side effects (weight gain, bone loss, diabetes) mean it’s used briefly and tapered fast.
For long-term control, immunosuppressants are key. Mycophenolate (CellCept) is now first-line for lupus nephritis, with 60-70% of patients achieving kidney response. Azathioprine (Imuran) and cyclophosphamide are older options still used when needed. Rituximab (Rituxan), which targets B-cells, helps when other drugs fail.
In 2021, the FDA approved anifrolumab, a new biologic that blocks type I interferon-a key driver of lupus inflammation. In trials, it reduced disease activity by 40-50%. It’s not for everyone, but it’s a major step forward.
What’s Next in Lupus Treatment?
The future of lupus care is precision medicine. Researchers are now looking at biomarkers to predict who will flare, who will respond to which drug, and who’s at risk for organ damage.
JAK inhibitors (like baricitinib) and BTK inhibitors, originally developed for other autoimmune diseases, are in phase III trials for SLE. Early results show 30-50% improvement in symptoms compared to placebo. These could become oral alternatives to biologics.
Another focus: clearing cellular debris. In lupus, dead cells aren’t removed properly, triggering immune attacks. New drugs aim to fix this cleanup process. It’s not just about suppressing the immune system anymore-it’s about restoring balance.
Living With Lupus: Daily Management
Managing lupus isn’t just about pills. It’s about lifestyle.
Sun protection is non-negotiable. Wear UPF 50+ clothing, avoid midday sun, and reapply sunscreen every two hours-even on cloudy days.
Exercise is medicine. Controlled studies show 65% of patients feel less fatigue after regular aerobic activity-walking, swimming, cycling-even just 30 minutes three times a week.
Sleep matters more than you think. Poor sleep worsens pain and inflammation. Aim for 7-8 hours. If you can’t sleep, talk to your doctor-lupus-related insomnia is treatable.
Heart health is critical. People with lupus have a 2-5 times higher risk of heart attack. Control blood pressure, cholesterol, and don’t smoke. Statins are often recommended, even if cholesterol levels are normal.
Monitoring saves lives. Blood tests every 3 months for kidney function (creatinine, urine protein) catch damage early. Regular blood counts check for infections or anemia. If your white blood cell count drops, you’re more vulnerable-so avoid crowds during flu season.
Prognosis: What to Expect
The good news? Most people with lupus live long lives. 80-90% survive at least 10 years with proper care. But survival isn’t the same as quality of life.
Those with lupus nephritis have a 10-year survival rate of 88%-still good, but lower than the 94% for those without kidney involvement. The biggest killers? Heart disease (30-40% of deaths), infections (20-25%), and active disease (10-15%).
Disparities are stark. Black and Hispanic patients are 2-3 times more likely to die from lupus than White patients. They’re also more likely to develop severe kidney disease earlier. Access to care, genetic factors, and social stressors all play roles.
Childhood-onset lupus affects about 20% of patients. These kids often have more aggressive disease-80% have major organ involvement at diagnosis. But with early, aggressive treatment, outcomes have improved dramatically.
When to Seek Immediate Help
Not every flare needs the ER. But these signs do:
- Chest pain that worsens with breathing (could be pericarditis or pulmonary embolism)
- Sudden confusion, seizures, or vision changes (neurological flare)
- Swelling in legs, foamy urine, or high blood pressure (kidney flare)
- Fever over 101°F with no clear cause (could be infection or active disease)
- Severe headache with vomiting or stiff neck (meningitis risk)
If you have any of these, go to urgent care or the ER. Delaying care can mean permanent damage.
Can you outgrow lupus?
No, lupus is a lifelong condition. It doesn’t go away, but it can go into remission-meaning symptoms are under control with little to no treatment. Some people stay in remission for years. But even then, the immune system remains primed to react. Stopping medication without medical supervision often leads to a flare.
Is lupus hereditary?
Lupus isn’t directly inherited like a genetic disease, but having a close relative with lupus or another autoimmune condition (like rheumatoid arthritis or thyroid disease) increases your risk. Over 50 genes are linked to higher susceptibility. But genes alone aren’t enough-you need an environmental trigger, like UV light or an infection, to set it off.
Can you have lupus without a rash?
Yes. While the butterfly rash is famous, many people never develop it. Some only have joint pain, fatigue, or kidney issues. Others get skin rashes in hidden areas-like the scalp or chest-that go unnoticed. Diagnosis relies on a combination of symptoms, blood tests, and organ involvement-not just skin signs.
Does hydroxychloroquine cure lupus?
No, it doesn’t cure lupus. But it’s the most important drug for most patients. It reduces flares by half, protects organs, lowers the risk of blood clots, and improves survival. It takes weeks to months to work fully. Stopping it-even if you feel fine-doubles your flare risk. It’s not optional; it’s foundational.
Can women with lupus have safe pregnancies?
Yes-but only if lupus is well-controlled before conception. Ideally, you should be in remission for at least 6 months. Certain medications, like mycophenolate and cyclophosphamide, are dangerous during pregnancy and must be switched out months in advance. Hydroxychloroquine is safe and recommended. With careful planning and monitoring, most women with lupus deliver healthy babies.
Are there natural remedies that help lupus?
No supplement or herb has been proven to control lupus. Omega-3s, vitamin D, and turmeric may help with general inflammation, but they don’t replace medication. Some herbal products can actually trigger flares or interact with drugs. Always talk to your rheumatologist before taking anything-even "natural" supplements.
What Comes Next?
If you’ve been diagnosed with lupus, your next step isn’t fear-it’s action. Find a rheumatologist who specializes in autoimmune diseases. Keep a symptom journal. Track your sun exposure, stress levels, sleep, and medications. Ask about your antibody profile and kidney function. Get vaccinated-flu, pneumonia, and COVID shots are critical. Avoid smoking. Stay active. Eat well. And remember: you’re not alone. With the right care, most people with lupus live full, meaningful lives.






It’s not a disease-it’s a cosmic glitch. Our immune system’s just tired of playing nice. We evolved to fight bacteria, not our own collagen. Maybe lupus is evolution’s way of saying, ‘You’ve gone too far with processed food and WiFi.’
Wait-so you’re telling me the government didn’t invent lupus to control the population? I’ve seen the patterns. 90% fatigue? That’s exactly how they make people docile. And hydroxychloroquine? Same drug they used in the 2020 pandemic panic. Coincidence? I think not.
Oh wow. Another American article pretending lupus is ‘manageable.’ In India, we don’t have ‘annual eye exams’ or ‘biologics.’ We have chai, prayer, and silence. You people treat symptoms like they’re optional accessories. Pathetic.
I’ve been living with this for 14 years… and I keep thinking: what if we’re not supposed to ‘control’ lupus… but learn to listen to it? It’s not an enemy-it’s a messenger. The body isn’t broken; it’s screaming for alignment. Sunlight? Stress? These aren’t triggers-they’re mirrors. Maybe the real treatment is stillness…
…and yet, I still take my Plaquenil. Because sometimes, the body needs both science and surrender.
I got lupus after my divorce. Coincidence? Nah. My ex was toxic. My body just gave up. Now I take pills, wear sunscreen like a zombie, and avoid people who say ‘just chill.’
You’re not alone. I’ve been in remission for 5 years. Some days are rough, but I walk, I sleep, I take my meds. You’ve got this.
For anyone new to this: hydroxychloroquine isn’t optional. It’s your anchor. I skipped it for 3 months after I ‘felt fine.’ Flare hit like a truck. Don’t be me. Take it. Even on vacation. Even when you’re mad at your doctor.
Western medicine is a scam. In India, we cure lupus with turmeric, yoga, and cow urine. You people pay $10,000 for a pill while we have millennia of wisdom. Why are you still reading this? Go drink some gomutra.
Technically, the term ‘lupus’ derives from the Latin word for wolf, referencing the facial lesion’s wolf-bite appearance-though this etymology is often misattributed to medieval physicians who believed it was caused by demonic possession. Modern immunology, however, has conclusively demonstrated the role of type I interferonopathy and neutrophil extracellular traps (NETs) in pathogenesis. The 2019 ACR/ELR criteria are, in fact, the most sensitive and specific classification tool to date-though they still underrepresent non-European populations. Your ‘journaling’ is statistically insignificant without biomarker correlation.
Thank you for this comprehensive and clinically accurate overview. I appreciate the inclusion of both pharmacological and lifestyle interventions. It’s refreshing to see a piece that balances scientific rigor with human experience.
Interesting. I’ve had lupus since 2010. Never got the butterfly rash. Just chronic fatigue and kidney issues. I didn’t know about the 90% statistic. That’s… accurate. I didn’t realize how common it was.
So… if anifrolumab blocks type I interferon, and interferon is what makes your body attack itself… does that mean lupus is basically your immune system having a really bad, overactive Zoom meeting? Like, everyone’s yelling, no one’s listening, and the host forgot to mute the mic?
Also-has anyone tried fasting? I’ve heard it resets immune cells. Not saying it’s magic. But… what if we’re overdrugging and under-listening?