Irritable Bowel Syndrome: How the Gut-Brain Axis Causes Symptoms and How to Find Relief
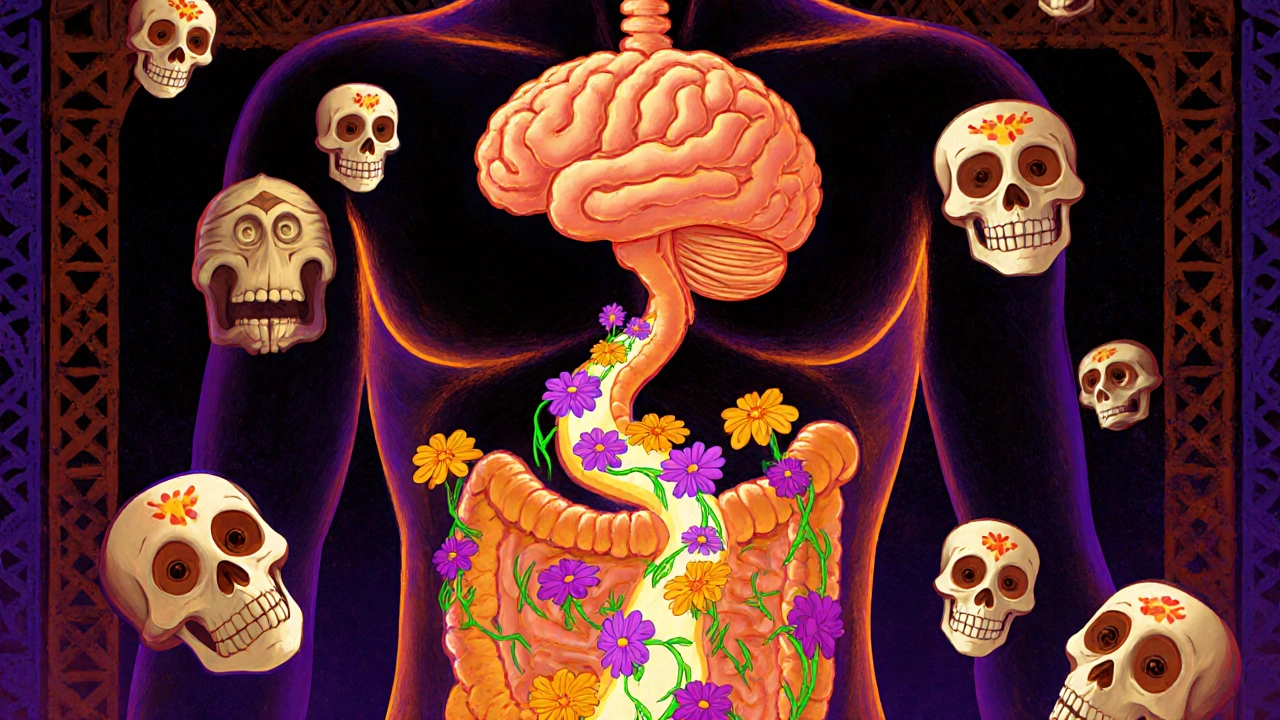
For millions of people around the world, stomach pain, bloating, and erratic bowel habits aren’t just annoying-they’re life-limiting. Irritable Bowel Syndrome (IBS) affects between 5% and 10% of the global population, yet most people still think of it as a simple digestive glitch. That’s outdated. Today, science shows IBS isn’t a gut problem alone-it’s a breakdown in communication between your gut and your brain. And understanding that connection is the key to real relief.
What IBS Really Is (And What It Isn’t)
IBS isn’t an infection, an allergy, or a structural issue like Crohn’s disease. It’s a functional disorder, meaning your organs look normal on scans, but they don’t work right. The Rome IV criteria, used by doctors worldwide since 2016, define IBS as recurrent abdominal pain at least one day a week over three months, linked to bowel movements or changes in stool frequency or form. But here’s what most doctors don’t tell you: about 76% of people with IBS also feel constant, dull discomfort-not sharp pain. And 60-70% have anxiety or depression. These aren’t coincidences. They’re part of the same system.
For decades, IBS was treated like a bowel motility problem. Loperamide for diarrhea, laxatives for constipation, antispasmodics for cramps. They helped a little, but never fixed the root. Now we know: the problem isn’t just your intestines. It’s the constant back-and-forth chatter between your gut and your brain. This is called the gut-brain axis (GBA). It’s a two-way highway made of nerves, hormones, and immune signals. When it gets noisy or broken, your gut reacts with pain, bloating, or sudden urges-even when there’s no infection or damage.
The Gut-Brain Axis: How Your Belly Talks to Your Head
Your gut has its own nervous system-called the enteric nervous system (ENS)-with over 100 million neurons. That’s more than your spinal cord. These nerves connect directly to your brain via the vagus nerve, the body’s longest cranial nerve. They also talk through hormones like serotonin and cortisol, and through immune cells that respond to what’s in your gut.
Here’s the shocking part: 95% of your body’s serotonin is made in your gut, not your brain. Serotonin controls bowel movements, pain signals, and even mood. In people with diarrhea-predominant IBS (IBS-D), gut serotonin levels are nearly 60% higher than in healthy people. In constipation-predominant IBS (IBS-C), serotonin is too low. That’s why drugs like alosetron (for IBS-D) and prucalopride (for IBS-C) work-they target serotonin receptors in the gut.
Brain scans reveal even more. People with IBS have thicker gray matter in areas that process pain and emotion, like the hypothalamus. At the same time, areas that help regulate emotions and decision-making, like the prefrontal cortex, are thinner. This isn’t because they’re “stressed out.” It’s because their brains have literally rewired themselves to be hypersensitive to gut signals. Think of it like a smoke alarm that goes off every time someone lights a candle-even when there’s no fire.
Why Your Microbiome Matters
Your gut is home to trillions of bacteria. In IBS, the balance is off. Studies show lower levels of beneficial bacteria like Bifidobacterium and higher levels of inflammation-triggering microbes. The ratio of Firmicutes to Bacteroidetes is often skewed. These bugs don’t just digest food-they produce chemicals that directly affect your brain. Short-chain fatty acids (SCFAs), for example, calm inflammation and help regulate your stress response. When these are low, your brain becomes more reactive to gut signals.
One probiotic strain, Bifidobacterium infantis 35624, has been shown in clinical trials to reduce bloating, pain, and bowel irregularity in 30-40% of IBS patients. That’s better than most over-the-counter meds. Fecal microbiota transplants (FMT) have shown promise too, but results vary wildly depending on the donor. It’s not a magic bullet, but it proves: your gut bugs are part of the problem-and part of the solution.
Dietary Changes That Actually Work
The low-FODMAP diet is the most studied and effective dietary approach for IBS. FODMAPs are short-chain carbs found in wheat, onions, garlic, dairy, apples, and artificial sweeteners. They’re poorly absorbed and ferment fast in the gut, pulling in water and producing gas. That distends the bowel, triggering pain in a hypersensitive system.
Studies show 50-76% of IBS patients get significant relief on this diet. But it’s not easy. The elimination phase lasts 4-6 weeks. You have to avoid onions, garlic, beans, milk, honey, and even some fruits. Many people quit because it’s too restrictive. The key? Do it with a dietitian. A 2022 survey of 45,000 IBS patients found those who worked with a professional had 25% better symptom improvement than those who went it alone.
After elimination, you slowly reintroduce foods one at a time to find your triggers. This isn’t about forever avoiding everything. It’s about learning what you can tolerate. Most people end up with a personalized diet that’s far less strict than the full elimination phase.

Neuromodulation: Rewiring Your Brain’s Response
What if you could teach your brain to stop overreacting to normal gut signals? That’s what gut-directed hypnotherapy does. It’s not stage hypnosis. It’s a structured, evidence-based therapy where you learn to visualize your gut as calm and controlled. In randomized trials, 70-80% of IBS patients saw major symptom improvement-double the rate of standard medication. And the effects lasted at least six months.
Another emerging option is transcutaneous vagus nerve stimulation (tVNS). You wear a small device behind your ear that sends gentle electrical pulses to the vagus nerve. Early studies show 45-55% reduction in abdominal pain. It’s non-invasive, affordable, and gaining FDA approval for IBS use.
Even cognitive behavioral therapy (CBT) helps-not because IBS is “all in your head,” but because it teaches your brain to respond differently to pain signals. One study found CBT improved IBS symptoms as much as medication, without side effects.
Medications: Targeting the Axis, Not Just Symptoms
Traditional IBS meds like antispasmodics or loperamide offer temporary relief but often come with side effects-drowsiness, constipation, dry mouth. Many patients stop taking them within three months.
Now, drugs are being designed to target the gut-brain axis directly:
- Alosetron (Lotronex): Blocks serotonin receptors in the gut. Works well for severe IBS-D in women, but carries a small risk of ischemic colitis. Requires strict monitoring.
- Prucalopride (Resolor): Boosts serotonin activity to speed up motility. Effective for IBS-C, with fewer side effects than older laxatives.
- Etrasimod: A new pill that modulates immune signaling. Phase III trials in 2023 showed 52% symptom improvement vs. 31% with placebo.
These aren’t cures, but they’re the first treatments that actually address the root mechanism-not just the symptoms.
Why Most People Struggle to Get Help
It takes an average of 3 to 7 years for someone with IBS to get diagnosed. Why? Because many doctors still treat it as a gut-only issue. Patients are told to “eat more fiber,” “cut caffeine,” or “just relax.” When that doesn’t work, they’re dismissed as anxious or depressed.
And even when they do get a diagnosis, access to effective treatments is limited. Gut-directed hypnotherapy requires a certified practitioner. There’s only one for every 500,000 people in rural areas. The cost? $1,200 to $2,500 for 7-12 sessions. Insurance rarely covers it.
Meanwhile, the low-FODMAP diet is hard to follow without expert guidance. Most online guides oversimplify the science. Patients end up eliminating too much or not enough. The result? Frustration, weight loss, and more anxiety.

What Works Best-And What to Avoid
Here’s what real-world data shows:
- Best for most people: Low-FODMAP diet + gut-directed hypnotherapy. Combined, they help over 80% of patients.
- Good for constipation: Prucalopride + fiber (soluble, like psyllium).
- Good for diarrhea: Alosetron (if severe) + bile acid binders like cholestyramine.
- Best for anxiety-linked IBS: CBT or mindfulness-based stress reduction.
- Avoid: Long-term use of loperamide, peppermint oil capsules (can worsen reflux), and unregulated probiotics without strain-specific evidence.
There’s no one-size-fits-all. But there is a proven path: start with education, then diet, then neuromodulation or targeted meds if needed.
The Future of IBS Treatment
In 2023, the first gut-brain axis biomarker panel-called VisceralSense™-hit the market. It measures 12 microbial metabolites and serotonin ratios to predict which treatment will work best for you. It’s not widely available yet, but it’s a sign of where things are headed: personalized medicine based on your unique gut-brain profile.
The NIH just launched a $15 million project to map individual gut-brain signatures and build AI-driven treatment algorithms. The European Union is funding a 4-year project to create the first full atlas of gut-brain signaling pathways.
By 2030, experts predict 45-50% of IBS treatment will target the gut-brain axis directly. Traditional symptom-only drugs will fade out. The future isn’t about suppressing pain. It’s about restoring communication.
Where to Start Today
If you have IBS, here’s your practical roadmap:
- Learn the gut-brain axis concept. Understanding it reduces fear and improves treatment adherence by 30%.
- See a registered dietitian for a low-FODMAP plan. Don’t guess-get guided.
- Ask your doctor about gut-directed hypnotherapy. Some hospitals offer it. Online programs like Nerva (approved by gastroenterologists) are affordable and effective.
- If symptoms persist, ask about serotonin-targeted meds or tVNS. Don’t settle for antispasmodics if they’re not working.
- Track your symptoms and triggers in a simple journal. Note food, stress, sleep, and bowel patterns. Patterns emerge over time.
IBS isn’t your fault. It’s not weakness. It’s a real, measurable disruption in your body’s communication system. The good news? We now have tools to fix it-not mask it. And the more you understand the gut-brain axis, the more power you have to take back control.
Is IBS just stress in the gut?
No. Stress doesn’t cause IBS, but it makes it worse. IBS is a real biological disorder involving changes in gut nerves, brain signaling, and gut bacteria. People with IBS have heightened sensitivity to normal gut activity. Stress can trigger flare-ups by activating the HPA axis and altering gut motility, but the root cause is physiological, not psychological.
Can probiotics cure IBS?
No single probiotic cures IBS. But specific strains like Bifidobacterium infantis 35624 have been shown in clinical trials to reduce bloating, pain, and bowel irregularity in 30-40% of patients. Most over-the-counter probiotics don’t contain these strains or aren’t dosed correctly. Look for products with clinically tested strains and CFU counts listed on the label.
How long does the low-FODMAP diet take to work?
Most people notice improvement within 2 to 6 weeks of starting the elimination phase. The full process-including reintroduction-takes 8 to 12 weeks. It’s not meant to be permanent. The goal is to identify your personal triggers so you can eat more freely without symptoms.
Is IBS linked to colon cancer?
No. IBS does not increase your risk of colon cancer, inflammatory bowel disease, or other structural gut diseases. However, symptoms like weight loss, blood in stool, or new-onset IBS after age 50 should be evaluated to rule out other conditions. Always discuss red flags with your doctor.
Can IBS go away on its own?
For some, symptoms improve over time with lifestyle changes, but IBS rarely disappears completely without intervention. Left untreated, it often becomes chronic. The good news is that with the right approach-diet, stress management, and targeted therapies-most people achieve long-term symptom control and return to normal daily life.







low FODMAP worked for me but only after i stopped being scared of eating fat.
after years of being told it was all in my head, i finally found a doctor who listened. the gut-brain connection isn't magic-it's biology. i wish i'd known this 10 years ago.
the fact that 95% of serotonin is made in the gut still blows my mind. no wonder antidepressants don't always fix IBS. we've been treating the symptom, not the source.
i've been managing my IBS for over 15 years and i can say with certainty that the combination of low-FODMAP and gut-directed hypnotherapy changed my life. i used to cancel plans weekly because i didn't know if i'd make it to the bathroom. now i travel internationally without anxiety. it's not a cure, but it's a path-and it's real. the science here is solid, and the emotional relief is just as important as the physical. don't let anyone tell you it's "just stress." your body is screaming, and we're finally learning how to listen.
has anyone tried tVNS? i'm curious if it's worth the investment or just another fad.
you're all missing the point. the microbiome studies are still preliminary. correlation isn't causation. and probiotics? most are marketing gimmicks with no peer-reviewed backing. don't believe the hype.
Wait-so you're telling me… that the gut has its own nervous system… with more neurons than the spinal cord… and serotonin is mostly produced there… and that the brain literally rewires itself in response?… and that’s why… traditional meds fail?… I’m not crying. You’re crying.
IBS isn't a disease you fight-it's a conversation you learn to have. Your gut isn't betraying you; it's trying to tell you something your brain forgot how to hear. The low-FODMAP diet? That's your dictionary. Hypnotherapy? That's your translator. And the science? It's finally translating the language your body's been speaking all along.
so you're telling me the solution to chronic pain is… therapy and a diet that makes you miss pizza? wow. groundbreaking.
the 80% success rate with low-FODMAP + hypnotherapy is cherry-picked. most studies have tiny samples, no long-term follow-up, and selection bias. also, who has $2,500 and 12 weeks to "learn to visualize their gut"? this reads like a wellness influencer’s dream, not medicine.
the real problem is that big pharma doesn't profit from diet and mindfulness. they want you hooked on pills. this article is a Trojan horse for anti-medical establishment propaganda. stick to science, not snake oil.
if you're reading this and struggling-i get it. i’ve been there. the low-FODMAP diet is brutal, but do it with a dietitian. and try Nerva-it’s $30/month and actually works. i didn’t believe it until my bloating vanished in 3 weeks. you’re not broken. you just need the right tools. 💪