Chronic Kidney Disease: How Early Detection Stops Progression

Most people with chronic kidney disease (CKD) don’t know they have it - until it’s too late. By the time symptoms like fatigue, swelling, or nausea show up, the kidneys have already lost a big chunk of their function. But here’s the truth: chronic kidney disease can be caught early, and when it is, you can stop it from getting worse. Not everyone will need dialysis. Not everyone will lose their kidneys. But only if you act before it’s advanced.
What Chronic Kidney Disease Really Means
Chronic kidney disease isn’t just about high creatinine or a single blood test. It’s defined by two things: kidney damage that lasts three months or more, and a drop in how well your kidneys filter waste. That’s measured by your eGFR - estimated glomerular filtration rate. If your eGFR is below 60 for more than 90 days, that’s a red flag. But here’s what most doctors don’t tell you: you can have normal eGFR and still have CKD. The real signal comes from your urine. Albumin, a protein your kidneys normally keep in your blood, starts leaking out when they’re damaged. That’s measured by the uACR - urine albumin-to-creatinine ratio. If your uACR is 30 mg/g or higher, you have kidney damage - even if your eGFR is still in the normal range. That’s stage 1 or 2 CKD. And it’s reversible, if you catch it fast. This two-test rule - eGFR AND uACR - is the gold standard. Yet, in 2022, over half of primary care providers still only checked creatinine. That’s like checking only one side of a coin. You’re missing 30-40% of early cases.Why Early Detection Saves Your Kidneys - and Your Life
CKD doesn’t just hurt your kidneys. It kills your heart. People with early-stage CKD are five times more likely to die from heart disease than from kidney failure. That’s why stopping progression isn’t just about preserving kidney function. It’s about staying alive. Studies show that catching CKD in stage 1 or 2 gives you a 5-7 year window to slow or even halt damage. In one major trial, patients with stage 2 CKD and proteinuria who started SGLT2 inhibitors (like dapagliflozin) cut their risk of kidney failure by 32%. That’s not a small number. That’s life-changing. Blood pressure control makes a huge difference too. If you keep your BP below 130/80 - not the old 140/90 target - you reduce your risk of kidney decline by 27%. That’s from the SPRINT trial, one of the most rigorous studies ever done on hypertension and kidneys. And it’s not just medication. Losing 5-10% of your body weight, cutting salt, and avoiding NSAIDs like ibuprofen can do the same work. A 2022 meta-analysis found that patients in structured early intervention programs saw their kidney function decline drop from 3.5 mL/min/year to just 1.2 mL/min/year. That’s a 66% improvement. It’s not magic. It’s consistency.Who Should Be Screened - And How Often
You don’t need to be sick to be at risk. Here’s who needs testing every year:- Anyone with type 1 or type 2 diabetes
- Anyone with high blood pressure
- People over 60
- Those with a family history of kidney failure
- African Americans, Native Americans, and Hispanic individuals - they’re 2 to 4 times more likely to develop CKD
- People on long-term NSAIDs, lithium, or certain antibiotics
The Two Tests That Matter
You need two tests. Not one. Not just a blood test. eGFR - This is calculated from your blood creatinine, age, sex, and race. But creatinine is flawed. It varies with muscle mass, diet, and even how much meat you ate the night before. Someone with low muscle mass - like an older woman or someone with chronic illness - can have normal creatinine but failing kidneys. That’s why cystatin C is now recommended in cases where creatinine looks normal but suspicion is high. uACR - This is a simple urine test. You pee in a cup. No fasting. No special prep. Just send it to the lab. A result of 30 mg/g or higher means protein is leaking out - your kidneys are damaged. A first-morning sample gives the most accurate reading. Both tests must be abnormal for at least three months to confirm CKD. That’s to rule out temporary things like dehydration or infection. But if both are off, you have CKD - and you need a plan.Stages of CKD - And What Each One Means
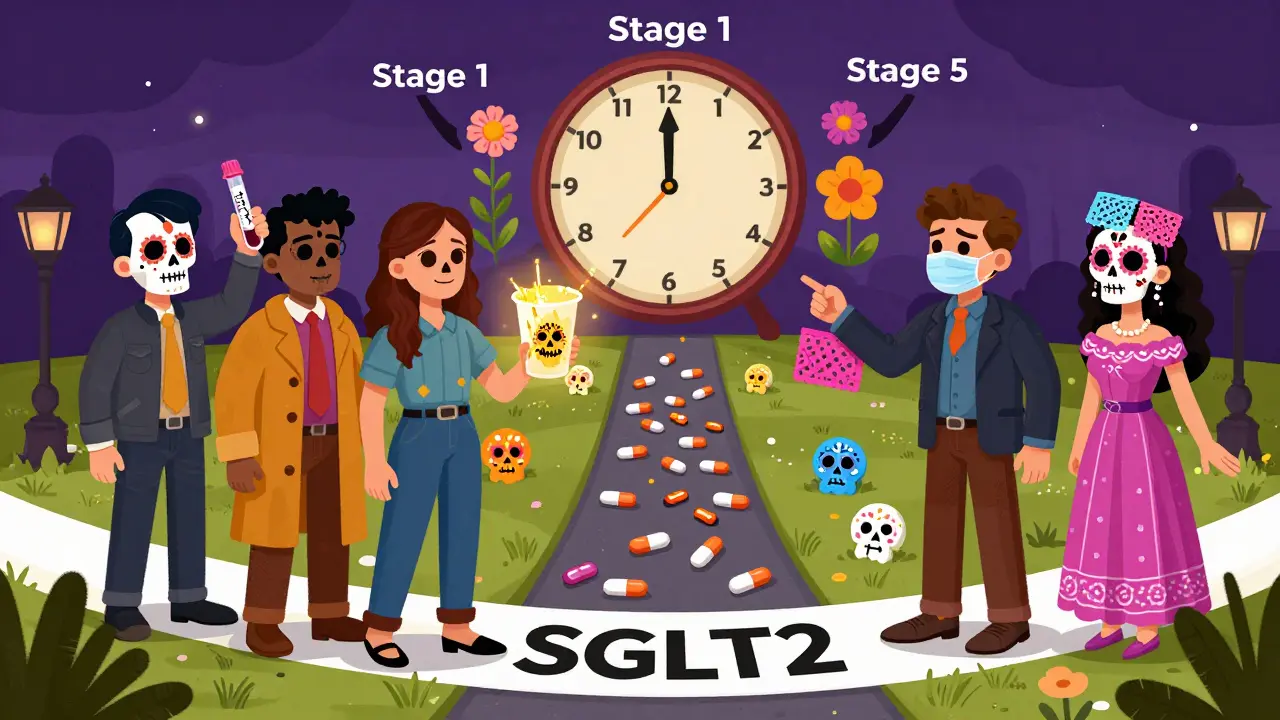
The staging system isn’t just labels. It’s your roadmap.- Stage 1: eGFR ≥90, uACR ≥30 - Kidneys are working fine, but damage is present. This is your wake-up call.
- Stage 2: eGFR 60-89, uACR ≥30 - Mild decline. Still early. Interventions work best here.
- Stage 3a: eGFR 45-59 - Mild to moderate loss. Time to get serious about meds and diet.
- Stage 3b: eGFR 30-44 - Moderate to severe. Risk of complications rises sharply.
- Stage 4: eGFR 15-29 - Severe loss. Prep for dialysis or transplant.
- Stage 5: eGFR <15 - Kidney failure. Requires dialysis or transplant.
What Works - And What Doesn’t
Here’s what actually slows CKD:- SGLT2 inhibitors - Originally diabetes drugs, now proven to protect kidneys even in non-diabetics.
- ACE inhibitors or ARBs - These blood pressure meds reduce protein leakage and are first-line for CKD with albuminuria.
- Low-sodium, low-protein diet - Cutting salt to under 2,300 mg/day and reducing animal protein helps. Not extreme - just smart.
- Stopping NSAIDs - Ibuprofen, naproxen, even high-dose aspirin can wreck kidneys over time.
- Regular exercise - Just 150 minutes a week of walking or cycling improves blood flow to kidneys.

Why So Many Cases Are Missed
It’s not just patient ignorance. The system fails too. In rural clinics, 68% of providers don’t order both tests. Electronic health records often don’t prompt for uACR. One Reddit user shared: “My doctor checked creatinine for 10 years. When they finally did uACR, I was stage 3.” Another problem: race adjustment in eGFR formulas. For decades, labs added 15% to the eGFR of Black patients, assuming they had more muscle mass. That meant many Black patients with early CKD were labeled “normal.” New guidelines are dropping this adjustment - and early detection in African Americans could rise by 12%. The U.S. Preventive Services Task Force still says there’s “insufficient evidence” to screen the general public. That’s outdated. With 1 in 7 Americans having CKD and $120 billion spent yearly on kidney care, this isn’t a debate - it’s a crisis.What You Can Do Right Now
If you’re at risk - and you probably are if you’re over 40, diabetic, or hypertensive - here’s your action plan:- Ask your doctor for an eGFR and uACR test - together. Don’t accept one without the other.
- If your uACR is above 30, ask about SGLT2 inhibitors or ACE/ARB meds. Don’t wait for your eGFR to drop.
- Get your blood pressure under 130/80. Use a home monitor. Track it.
- Stop NSAIDs. Use acetaminophen for pain instead.
- Reduce salt. Cook at home. Avoid processed food.
- Ask for a kidney health chart. Studies show patients who see their stage visually are 28% more likely to stick to their plan.
What’s Changing in 2025
The game is shifting. In 2023, the FDA cleared the first AI tool - NephroSight - that predicts CKD risk before eGFR drops. It uses 32 data points: blood pressure, cholesterol, HbA1c, even sleep patterns. It’s being rolled out in VA hospitals. The Biden administration is funding $150 million to make dual testing mandatory in all federally funded clinics by 2026. That could catch 1.2 million new cases. Point-of-care uACR tests - the kind you can do in a doctor’s office in 10 minutes - are coming to market in 2025. Imagine getting your results while you’re still in the chair. This isn’t science fiction. It’s happening. And the people who benefit most? Those who get tested now - before the system catches up.Can chronic kidney disease be reversed?
In early stages (1 and 2), yes - damage can be slowed or even partially reversed with medication, diet, and blood pressure control. Once you reach stage 3 or beyond, the focus shifts to preventing further decline. The goal isn’t always full recovery - it’s avoiding dialysis.
Is a urine test really enough to detect kidney damage?
Yes - the urine albumin-to-creatinine ratio (uACR) is the most sensitive early marker of kidney damage. It detects protein leakage before the kidneys’ filtering ability drops. Blood tests alone miss up to 40% of early cases.
Why do I need both eGFR and uACR if my blood work looks normal?
Because eGFR measures how well your kidneys filter, but uACR shows if they’re leaking. You can have normal filtering but still have damaged filters - like a sieve with holes. That’s why both are needed. One test alone isn’t enough.
Can I get tested without a doctor’s order?
In most cases, no. These tests require a lab order. But some pharmacies and community health centers in Australia and the U.S. now offer free or low-cost CKD screening events - especially during National Kidney Month in March. Ask your local clinic.
Are there side effects from the medications used to slow CKD?
SGLT2 inhibitors can cause genital yeast infections or mild dehydration. ACE inhibitors may cause a dry cough or high potassium. But these are manageable. The risks of untreated CKD - heart attack, stroke, dialysis - are far greater. Always discuss side effects with your doctor.
If I have diabetes, how often should I get tested?
Annually - starting at diagnosis for type 2 diabetes, and five years after diagnosis for type 1. Don’t wait for symptoms. Kidney damage can begin within the first year of diabetes.
Does drinking more water help my kidneys?
Not if you’re already healthy. For people with CKD, forcing extra water doesn’t help and can even be harmful if you have fluid retention. Drink when you’re thirsty. Don’t overdo it. The real fix is controlling blood pressure and sugar - not water intake.
Can I still eat meat if I have early-stage CKD?
Yes - but limit it. Aim for 0.6 to 0.8 grams of protein per kilogram of body weight. That’s about 4-5 ounces of meat per day for most people. Swap some meat for plant proteins like beans, lentils, and tofu. It reduces kidney strain and helps control blood pressure.






Just got my uACR back last week - 42 mg/g. eGFR was fine. I asked my doc about SGLT2 inhibitors and she actually knew what I was talking about. Started on dapagliflozin. No side effects yet. Feeling better already. This post saved me from waiting until I was stage 3.
Let’s be real - if your doctor isn’t ordering both tests, they’re practicing medicine from 2005. The fact that half of primary care docs still ignore uACR is a systemic failure, not a patient problem. You don’t need a PhD to understand that protein in urine = broken filter. But you do need a doctor who cares enough to look.
I’m 52, diabetic since 2018, and never had a uACR until last month. Turned out I was stage 2. My doctor didn’t even mention it until I brought it up. This is why education matters - not just for patients, but for providers too. Thank you for laying this out so clearly.
If you’re over 40 and have high blood pressure or diabetes - don’t wait. Ask for the two tests. Write it down. Bring it to your appointment. You’re not being difficult - you’re being smart. And if your doctor pushes back, find one who doesn’t. Your kidneys won’t wait.
The notion that 'early detection saves kidneys' is a gross oversimplification. The data cited is cherry-picked from trials with highly controlled populations. Real-world adherence to SGLT2 inhibitors is abysmal. Most patients stop due to cost, side effects, or lack of follow-up. The 66% decline in eGFR loss? That’s in a clinical trial, not your local Walgreens clinic. This post reads like pharmaceutical marketing dressed as public health advice.
They want you to get tested so they can sell you drugs. Who profits from all this screening? Big Pharma. The VA’s AI tool? Probably built by Lockheed. They’re scared you’ll figure out that kidney failure is just another way to make you pay for medicine. Drink lemon water. Stop trusting the system.
My uncle was on dialysis for 8 years and he ate junk food his whole life. He also smoked. So what’s the point of all this testing if some people just get sick no matter what? I’m not getting tested because I don’t want to stress over numbers. Life’s too short. Let the doctors handle it.
India has 80 million diabetics. Less than 5% get uACR tested. Why? Because doctors don’t have time, labs don’t have kits, and patients can’t afford it. Your ‘gold standard’ doesn’t exist in rural clinics. You’re preaching to the urban elite. The real crisis isn’t lack of awareness - it’s lack of infrastructure.
Just got my results back - uACR 38 😔 I’ve been ignoring my BP for years. Time to start walking, cut the chips, and ask my doc about the SGLT2 med. Thanks for the nudge. I’ve got this 💪
As someone who grew up in a family where kidney disease was common, I’ve seen what happens when you wait. My mom was diagnosed at stage 4. She’s on dialysis now. If we’d known earlier - she’d still be gardening. This isn’t theoretical. It’s personal. Please, if you’re at risk - get tested. Now.
Australia dropped 22% in end-stage disease? Yeah, because they have a national health system. In the US, you need insurance, a doctor, transportation, time off work, and money for copays. This isn’t about awareness - it’s about class. Your ‘action plan’ only works if you’re middle class and white. For the rest of us? Good luck.
This is one of the most comprehensive, evidence-based summaries of early CKD detection I’ve ever seen. The distinction between eGFR and uACR is critical, and the emphasis on stage 1-2 intervention is spot-on. The data on SGLT2 inhibitors and BP targets is meticulously cited. This should be required reading for all primary care providers. Thank you for the clarity and rigor.
They say AI predicts CKD before eGFR drops? That’s just fancy statistics. What’s next - predicting your death from your Spotify playlist? And why is the government spending $150 million on this? Maybe they should fix the water supply instead. I’ve heard kidney disease is caused by fluoride. Or maybe it’s 5G. Either way, I’m not getting tested until they stop lying to us.
My uACR was 45 last year. I didn’t do anything. This year it’s 52. I’m not on meds. I don’t care. I’ve had kidney pain since I was 18. I’m 41 now. Maybe I’m just built different. Or maybe the tests are wrong. Either way, I’m not letting doctors scare me into taking pills I don’t need.
Hey Frank - I saw your comment. I’m the one who started the SGLT2. You’re right - it’s not perfect. But I’ve lost 12 lbs, my BP dropped to 126/78, and my uACR went from 42 to 28 in 4 months. It’s not magic. It’s consistency. I’m not ‘cured’ - but I’m not heading to dialysis either. You’re not alone in this.