How to Reduce Opioid Withdrawal: Symptoms, Support, and Science
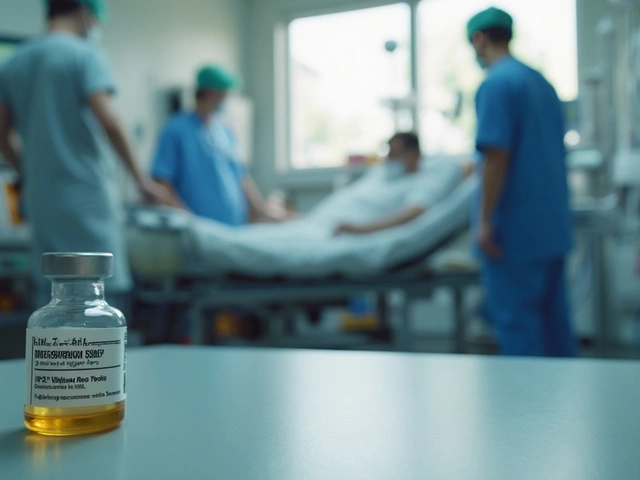
When someone stops using opioids, the body reacts—often violently. opioid withdrawal, the physical and emotional response when opioid use is reduced or stopped. Also known as opioid detox syndrome, it’s not just about feeling sick—it’s a complex neurological reset that can last days or weeks. This isn’t weakness. It’s biology. Opioids change how your brain handles pain, mood, and stress. When they’re gone, your nervous system scrambles to catch up. That’s why cold turkey often fails. Most people need help to reduce opioid withdrawal safely and stay off drugs long-term.
There are three main ways to manage this: medication-assisted treatment, using FDA-approved drugs like methadone, buprenorphine, or naltrexone to ease cravings and symptoms, support systems, counseling, peer groups, and family involvement that rebuild emotional stability, and opioid withdrawal symptoms, the physical signs like nausea, muscle aches, anxiety, and insomnia that make quitting feel impossible. You can’t ignore any of these. Medication alone won’t fix the mental habits. Therapy alone won’t calm the shaking hands. You need both. And timing matters—starting support before withdrawal peaks makes a huge difference.
People who try to quit without help often relapse within days. That’s not because they lack willpower. It’s because withdrawal triggers intense cravings and physical discomfort. Studies show that using buprenorphine reduces withdrawal severity by up to 70% compared to no treatment. Adding counseling cuts relapse rates in half. Even simple things—staying hydrated, eating regular meals, getting light exercise—help your body recover faster. This isn’t about willpower. It’s about giving your body the tools to heal.
What you’ll find below are real, practical guides written by people who’ve been through this. From how to talk to your doctor about MAT options, to what over-the-counter remedies actually help with muscle cramps, to how to handle sleepless nights without pills. These aren’t theory pieces. They’re field reports from patients, pharmacists, and clinicians who’ve seen what works—and what doesn’t. No fluff. No slogans. Just what you need to know to get through it.

Learn how to safely reduce opioid use with a step-by-step guide to minimize withdrawal symptoms, avoid overdose risks, and improve long-term health. Evidence-based strategies for patients and providers.
Chris Gore Dec 1, 2025