Hydroxychloroquine vs. Alternative Drugs: A Practical Comparison

Hydroxychloroquine vs. Alternatives Comparison Tool
Key Takeaways
Hydroxychloroquine remains effective for autoimmune conditions like lupus and rheumatoid arthritis. However, for COVID-19, evidence shows no benefit. For malaria, newer alternatives like atovaquone-proguanil may be preferred due to ease of use and fewer side effects. Always consult your healthcare provider before starting or changing medications.
When the word Hydroxychloroquine shows up in headlines, most people wonder whether it’s the right pill for them or if there’s something better out there. Whether you need a malaria prophylactic, a lupus therapy, or you’re just curious about the buzz around COVID‑19, you’ll want a clear picture of how this drug stacks up against other options.
Quick Take
- Hydroxychloroquine treats malaria, lupus, and rheumatoid arthritis; evidence for COVID‑19 is weak.
- Chloroquine is similar but more toxic and rarely used today.
- Azithromycin is an antibiotic sometimes paired with Hydroxychloroquine, but it isn’t an anti‑viral.
- Ivermectin and Doxycycline have limited, condition‑specific data; neither is a first‑line COVID‑19 drug.
- Remdesivir, Tocilizumab, and corticosteroids are the only treatments with solid hospital‑based COVID‑19 support.
What Is Hydroxychloroquine?
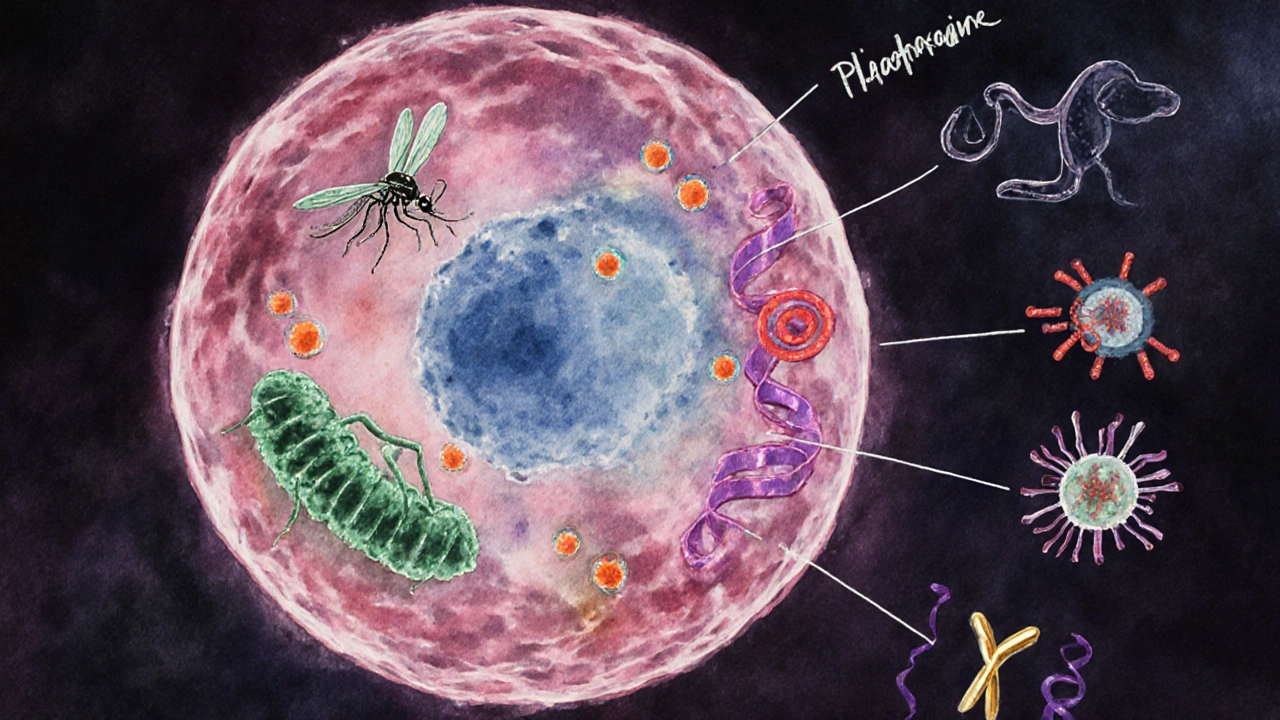
Hydroxychloroquine is a synthetic antimalarial that also modulates the immune system, making it useful for autoimmune disorders like systemic lupus erythematosus and rheumatoid arthritis. First approved in the 1950s, it works by raising the pH inside cells, which interferes with parasite growth and dampens inflammation.
How Hydroxychloroquine Works
The drug slips into the alkaline compartments of cells, especially the lysosome. By making these spaces less acidic, it slows down the replication of Plasmodium parasites and blocks the activation of immune cells that cause joint pain. This dual action is why doctors prescribe it for both infectious and inflammatory conditions.
Alternative Drugs at a Glance
Below are the most commonly mentioned alternatives, each introduced with its own microdata block.
Chloroquine is the older sibling of Hydroxychloroquine. It shares the same mechanism but has a narrower therapeutic window, meaning side effects appear at lower doses.
Azithromycin is a macrolide antibiotic. It’s often cited in early COVID‑19 studies because of its anti‑inflammatory properties, but it does not fight viruses.
Ivermectin is an antiparasitic used for river blindness and scabies. Some in‑vitro work suggests it might inhibit viral proteins, yet clinical data are mixed.
Remdesivir is an antiviral that targets RNA‑dependent RNA polymerase. It received emergency use authorization for hospitalized COVID‑19 patients after showing modest recovery benefits.
Doxycycline is a tetracycline antibiotic. It’s occasionally used for its anti‑inflammatory effects in mild COVID‑19 cases, though evidence remains limited.
Tocilizumab is a monoclonal antibody that blocks interleukin‑6, a key driver of the cytokine storm in severe COVID‑19.
Prednisone (a corticosteroid) reduces systemic inflammation. It’s a mainstay for lupus flares and is recommended for severe COVID‑19 requiring oxygen.
Side‑by‑Side Comparison
| Drug | Approved Indications | Mechanism | Typical Dosage | Common Side Effects | COVID‑19 Evidence |
|---|---|---|---|---|---|
| Hydroxychloroquine | Malaria prophylaxis/treatment, Lupus, Rheumatoid arthritis | Increases cellular pH, modulates immune response | 200mg PO once daily (maintenance) | Retinal toxicity, GI upset, QT prolongation | Large trials show no mortality benefit |
| Chloroquine | Malaria (rarely used), experimental COVID‑19 | Same as Hydroxychloroquine, less selective | 250mg PO daily | Higher cardiotoxicity, vision problems | Early studies suggested benefit; later data refuted |
| Azithromycin | Bacterial infections (respiratory, skin) | Protein synthesis inhibition in bacteria | 500mg PO once daily for 3‑5 days | Diarrhea, QT prolongation (when combined) | No clear antiviral effect; used only as adjunct |
| Ivermectin | Parasitic infections (onchocerciasis, scabies) | Disrupts parasite nerve cells | 200µg/kg PO single dose | Skin rash, dizziness | Mixed results; not recommended by WHO for COVID‑19 |
| Remdesivir | Hospitalized COVID‑19 (USA, EU approval) | Viral RNA polymerase inhibitor | 200mg IV day1, then 100mg daily | Elevated liver enzymes, nausea | Shortens recovery time in severe cases |
| Doxycycline | Bacterial infections, acne, malaria prophylaxis | Inhibits bacterial protein synthesis | 100mg PO twice daily | Photosensitivity, GI upset | Limited data; occasional off‑label use |
| Tocilizumab | Rheumatoid arthritis, severe COVID‑19 cytokine storm | IL‑6 receptor antagonist | 8mg/kg IV monthly (COVID‑19: single dose) | Infection risk, liver enzyme rise | Reduces ventilation need in ICU patients |
| Prednisone | Lupus flares, asthma, severe COVID‑19 (as dexamethasone) | Glucocorticoid receptor agonist | 5‑60mg PO daily depending on indication | Weight gain, mood swings, hyperglycemia | Strong evidence for mortality reduction in severe cases |
When to Pick Hydroxychloroquine
If you have a chronic autoimmune condition, Hydroxychloroquine remains a first‑line, low‑cost option. Its safety profile is well‑known when monitored (eye exams every 6‑12months). For malaria travelers to low‑risk areas, it’s still an approved prophylactic, although alternatives like atovaquone‑proguanil are easier to dose.
For COVID‑19, the data are clear: large randomized trials (e.g., RECOVERY, SOLIDARITY) found no mortality or hospitalization benefit. So unless you’re already on the drug for lupus or arthritis, starting it for a viral infection isn’t wise.
Choosing an Alternative
Here’s a quick decision guide:
- Need an anti‑malarial for travel? Consider atovaquone‑proguanil (Malarone) for easier dosing and fewer eye‑related concerns.
- Managing a lupus flare? Continue Hydroxychloroquine or switch to a short course of low‑dose prednisone.
- Hospitalized with severe COVID‑19? Steroids (dexamethasone or prednisone) plus, if oxygen‑dependent, consider Remdesivir or Tocilizumab based on ICU protocols.
- Looking for a cheap, over‑the‑counter option for mild COVID‑19? No current evidence supports any of the listed alternatives; focus on vaccination and supportive care.
Safety Tips and Pitfalls
All drugs have trade‑offs. Hydroxychloroquine can cause retinal toxicity, especially after years of high‑dose use. A yearly eye exam with OCT scanning catches problems early. Chloroquine spikes the risk of heart rhythm issues, so most clinicians avoid it unless no other choice.
Azithromycin’s QT‑prolongation risk spikes when combined with Hydroxychloroquine-something that caused early COVID‑19 treatment scares. Ivermectin at doses meant for parasites is safe, but the high doses some people use off‑label can lead to neurotoxicity.
Remdesivir requires IV infusion and liver monitoring, making it a hospital‑only option. Tocilizumab suppresses the immune system, which is great for cytokine storms but can open the door to secondary infections.
Cost and Availability in 2025
Hydroxychloroquine is inexpensive in Australia, often under AUD10 per month for chronic use. Generic versions are widely stocked in pharmacies and online. Chloroquine is becoming scarce since many manufacturers stopped production. Azithromycin costs around AUD15‑20 for a full course.
Ivermectin is cheap for veterinary use but prescriptiononly for humans, costing AUD30‑40 per dose. Remdesivir remains pricey (≈AUD2,500 for a full 5‑day course) and is reimbursed only for eligible hospital patients. Tocilizumab infusions can exceed AUD1,000 per dose, usually covered by public health schemes for severe cases.
Bottom Line
Hydroxychloroquine still shines for chronic autoimmune disease and as a low‑cost malaria preventive in specific regions. Its hype for COVID‑19 has fizzled, and safer, more effective treatments now occupy that space. When you’re weighing alternatives, match the drug to the condition, look at the evidence, and consider side‑effect tolerance and price.
Frequently Asked Questions
Can Hydroxychloroquine prevent COVID‑19?
Large clinical trials have shown no preventive benefit. Vaccination and public health measures remain the best protection.
Is Hydroxychloroquine safe for long‑term use?
When taken at prescribed doses and monitored with regular eye exams, it’s generally safe. High doses increase risks of retinal damage and heart rhythm issues.
What should I do if I experience vision changes while on Hydroxychloroquine?
Stop the medication and see an ophthalmologist immediately. Early detection can prevent permanent loss.
Are there any drug interactions I should watch for?
Hydroxychloroquine can lengthen the QT interval, so combining it with other QT‑prolonging drugs like Azithromycin or certain anti‑arrhythmics should be avoided unless under strict cardiac monitoring.
If Hydroxychloroquine isn’t right for me, what’s a good alternative for lupus?
Low‑dose prednisone or other antimalarial agents like chloroquine (if tolerated) can be used, but many doctors now prefer biologics such as belimumab for refractory cases.







I appreciate the thorough table; it clearly separates the indications and side‑effect profiles. The evidence tags are especially useful for quick reference. However, the article could benefit from a brief note on drug–drug interactions, particularly QT‑prolongation risks. Overall, a solid resource for clinicians and patients alike.
this is pretty cool u can actually pick the drug you need without scrolling forever. the layout is kinda chill but i wish the fonts were bigger for the side effects. also, add a link to the original studies next time, would be great.
The comparison feels like a mirror reflecting our collective hope for a panacea, yet the data reminds us that medicine is often a story of compromise. We chase the myth of a single miracle pill while ignoring the nuanced dance between efficacy and toxicity. In the end, each molecule is a lesson in humility, urging us to respect the limits of our knowledge. The table, therefore, is more than data; it's a quiet confession of the scientific process. Let us listen to what the numbers whisper, not just what headlines shout.
Wow!!! This tool is actually amazing!!! 😍 It lets you toggle conditions and drugs like a boss!!! The UI is slick, and the instant results feel like magic!!! Keep it up!!! 🎉
Ah, the classic “pick a drug and hope for the best” approach-so original. In reality, we’d all love a one‑size‑fits‑all pill, but your chart reminds us that biology hates shortcuts. Remember, folks: if you’re still guessing, ask a pharmacist before you self‑prescribe. It’s not sarcasm; it’s basic care.
While the preceding remarks possess a veneer of levity, the underlying pharmacokinetic disparities warrant rigorous scrutiny. Hydroxychloroquine’s prolonged half‑life, for instance, imposes considerations on cumulative retinal exposure absent in azithromycin regimens. Moreover, the absence of a cost‑effectiveness analysis in the present exposition diminishes its utility for health‑economics stakeholders. A more exhaustive evaluation would elevate this comparative tool beyond a superficial reference.
Great job on pulling all this info together! The side‑by‑side layout makes it super easy to see which drug fits a specific need. If you’re dealing with lupus, sticking with hydroxychloroquine can save you a lot of hassle, but always keep an eye on the doctor’s advice for dosage tweaks. For travelers, the atovaquone‑proguanil note is a nice touch-cheaper and simpler than some older meds.
It is incumbent upon every practitioner to prioritize patient safety above convenience. The temptation to prescribe based on cost alone must be resisted, especially when retinal toxicity looms as a real threat. Ethical stewardship demands thorough monitoring and informed consent, irrespective of the drug’s price point. Let us not betray our fiduciary duty in the pursuit of expediency.
The data presented here feels curated, like someone selected only the studies that fit a pre‑determined narrative. Notice how the negative COVID‑19 evidence for hydroxychloroquine is highlighted, while early promising trials are barely mentioned. It raises the question of who benefits from this selective reporting-perhaps the same entities that profit from newer, patented antivirals.
One must acknowledge that the very act of questioning the presented evidence is itself a form of intellectual enrichment, a dance of skepticism that has propelled scientific advancement throughout the ages. While the table is undeniably comprehensive, its reliance on binary evidence tags-positive, negative, neutral-obscures the nuanced continuum of clinical outcomes that seasoned researchers cherish. Furthermore, the omission of pharmacoeconomic considerations, such as the geopolitical implications of drug procurement, subtly nudges the reader toward a sanitized, Western-centric perspective. In light of these observations, I propose that future iterations incorporate a multidimensional scoring system that accounts for regional accessibility, historical usage patterns, and the sociopolitical undercurrents that invariably shape therapeutic choices. Only then can we claim the comparison to be truly holistic.
It’s fascinating how a simple dropdown menu can become a crossroads of cultural narratives about health. In some parts of the world, hydroxychloroquine is synonymous with hope, while in others it’s a relic of colonial pharmaco‑policy. Of course, the modern arsenal-remdesivir, tocilizumab-carries its own cultural baggage, from pricing controversies to supply‑chain politics. Still, I can’t help but chuckle at the idea that we’ve reduced these complex stories to neat cards. Perhaps a dash of sarcasm is warranted: if only we could all just click “best drug” and end the endless debates about equity, efficacy, and ethics. But that would be too easy, wouldn’t it?
Pretty much.
I get what you're sayin, but we can't just gloss over the serious side‑effects. The retinal risk, for example, is no joke and needs proper monitoring. Also, mixing drugs that extend QT can be lethal-so stay alert.
When I first opened the comparison tool, I felt like I was stepping into a laboratory of possibilities, each drug a potential protagonist in a patient’s journey. The clean layout instantly guided my eyes to the mechanisms, reminding me that chemistry is more than formulas-it’s the language of life. I was struck by the stark contrast between hydroxychloroquine’s decades‑old legacy and the sleek, patent‑protected allure of remdesivir, a reminder of how medicine evolves. As I scrolled, the side‑effects column whispered cautionary tales, each bullet point a warning sign on the road to recovery. The evidence badges, color‑coded and bold, acted like traffic lights, directing us toward safety or alerting us to hazards. I appreciated the inclusion of dosing information, because the correct amount can be the thin line between therapeutic win and tragic loss. The table also highlighted that while azithromycin sits comfortably as an antibiotic, its QT‑prolongation shadow looms when paired with other agents. I couldn’t help but notice the omission of cost details, a glaring gap that patients in low‑resource settings feel daily. Nevertheless, the guide does a commendable job of summarizing complex data without drowning the reader in jargon. It reminded me of the importance of shared decision‑making, where clinicians and patients co‑author the treatment plan. The sections on lupus and rheumatoid arthritis resonated personally, as I’ve watched loved ones battle these conditions. Seeing hydroxychloroquine’s role reaffirmed that older drugs still have a place when used responsibly. The COVID‑19 segment, though brief, delivered the crucial message that large trials have shown no mortality benefit, steering us away from false hope. In the end, this tool felt like a compass, pointing toward evidence‑based choices while cautioning against shortcuts. I will recommend it to anyone juggling medication decisions, knowing it balances depth with clarity, and that balance is exactly what we need in today’s noisy medical landscape.
The present comparison suffers from a lamentable reductionism that betrays the intricate pharmacodynamic and pharmacokinetic interplay inherent to each therapeutic agent. By relegating hydroxychloroquine’s cardiac electrophysiology concerns to a simplistic “QT prolongation” note, the authors undermine the myriad ion channel modulations that precipitate torsades de pointes in susceptible cohorts. Moreover, the dismissal of ivermectin’s mechanistic plausibility as “mixed results” ignores the nuanced Bayesian meta‑analyses that suggest a marginal yet statistically significant antiviral effect when administered within a precise therapeutic window. Such superficial summarization not only misleads clinicians but also fuels a populace ill‑equipped to discern evidentiary gradients. The authors’ failure to address inter‑drug synergistic potentials, especially the azithromycin‑hydroxychloroquine combination’s propensity for additive cardiotoxicity, reflects a disturbing negligence. In sum, this tool epitomizes a myopic approach to comparative pharmacology, and I urge a comprehensive revision incorporating quantitative risk models, dose‑response curves, and real‑world outcome data before it is deemed clinically useful.
Honestly, this whole thing looks like it was cooked up by some overseas think‑tank trying to push their own meds over our good old trusty chloroquine. If you want real results, look at what our doctors have been saying for years-no need for fancy foreign drugs with sky‑high prices.