Lenalidomide — What You Need to Know
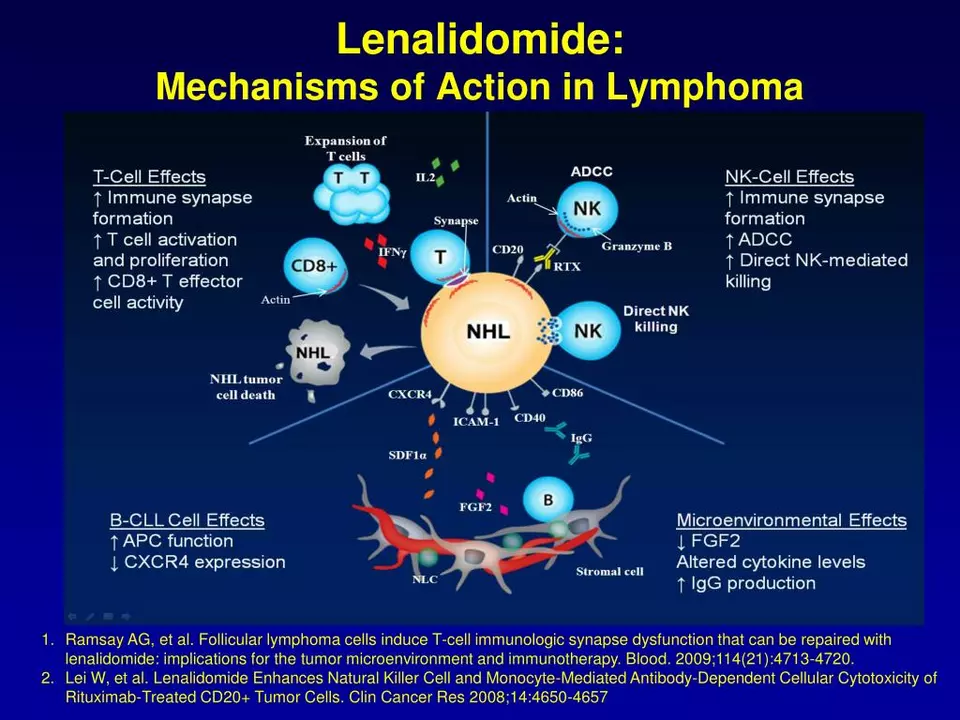
Lenalidomide is a prescription medicine used mainly to treat certain blood cancers and blood disorders. Doctors prescribe it for multiple myeloma, myelodysplastic syndromes, and mantle cell lymphoma in some cases. It works by changing how immune cells and blood vessels behave, which can slow cancer growth.
Before you start lenalidomide, your doctor will explain risks and benefits and do blood tests. This medicine can cause low blood counts, increasing the chance of infection, bleeding, or anemia. Regular blood work is essential so your doctor can adjust dose or pause treatment if needed.
Common side effects include fatigue, diarrhea, constipation, rash, and low white blood cells. More serious risks are blood clots and birth defects. Because of the high risk of severe birth defects, people who can become pregnant must follow strict pregnancy prevention programs and use effective contraception. Men should also use condoms during treatment and for a time after stopping the drug to avoid exposing partners.
How you take lenalidomide depends on your diagnosis and lab results. Doses vary widely; your healthcare team will give a schedule and tell you whether to take it with food. Never change dose on your own. If you miss a dose, contact your provider for guidance rather than doubling up.
Drug interactions matter. Tell your doctor about all medicines, supplements, and herbal products you use. Blood thinners, certain antibiotics, and drugs that affect blood counts can change lenalidomide safety. Your team may add medicines to prevent blood clots if you have higher clotting risk.
If you're worried about cost or access, ask your provider about patient assistance programs or manufacturer support. Some hospitals and clinics can help with paperwork for financial aid. Buying lenalidomide online without a prescription is risky and often illegal, and counterfeit products are common. Always use a licensed pharmacy and follow your prescriber's instructions.
Watch for warning signs and call your doctor right away for fevers, sudden shortness of breath, chest pain, heavy bleeding, severe rash, or signs of pregnancy. Keep a list of symptoms and lab dates so you can track how you're doing.
Questions you can ask your doctor: What is the goal of treatment? How long will I take lenalidomide? What tests will monitor side effects? What contraceptive rules apply to me? Can I get help with medication costs?
This tag page collects articles that relate to cancer drugs, buying medicines safely, and treatment alternatives. If you need more detail, talk to your oncologist or pharmacist — they can tailor advice to your condition and other medications.
Practical tips: keep a written medication calendar showing doses and lab dates, wear a medical ID if you have low blood counts, avoid live vaccines while on treatment, and store capsules in original packaging at room temperature away from moisture. Tell any dentist or surgeon you are taking lenalidomide before procedures. Ask your care team how long precautions continue after your last dose and whether you should use extra sun protection. Keep notes daily.
As a blogger, I recently came across the topic of lenalidomide's role in the treatment of POEMS syndrome. It's fascinating to learn that lenalidomide, an immunomodulatory drug, has shown promise in treating this rare and debilitating disorder. Studies have indicated that it can effectively improve symptoms and reduce disease progression. Moreover, lenalidomide's tolerability and safety profile make it a viable treatment option for patients who are not suitable for other therapies. In summary, lenalidomide is emerging as a potential game-changer in the battle against POEMS syndrome, offering patients hope for a better quality of life.
Chris Gore May 6, 2023




