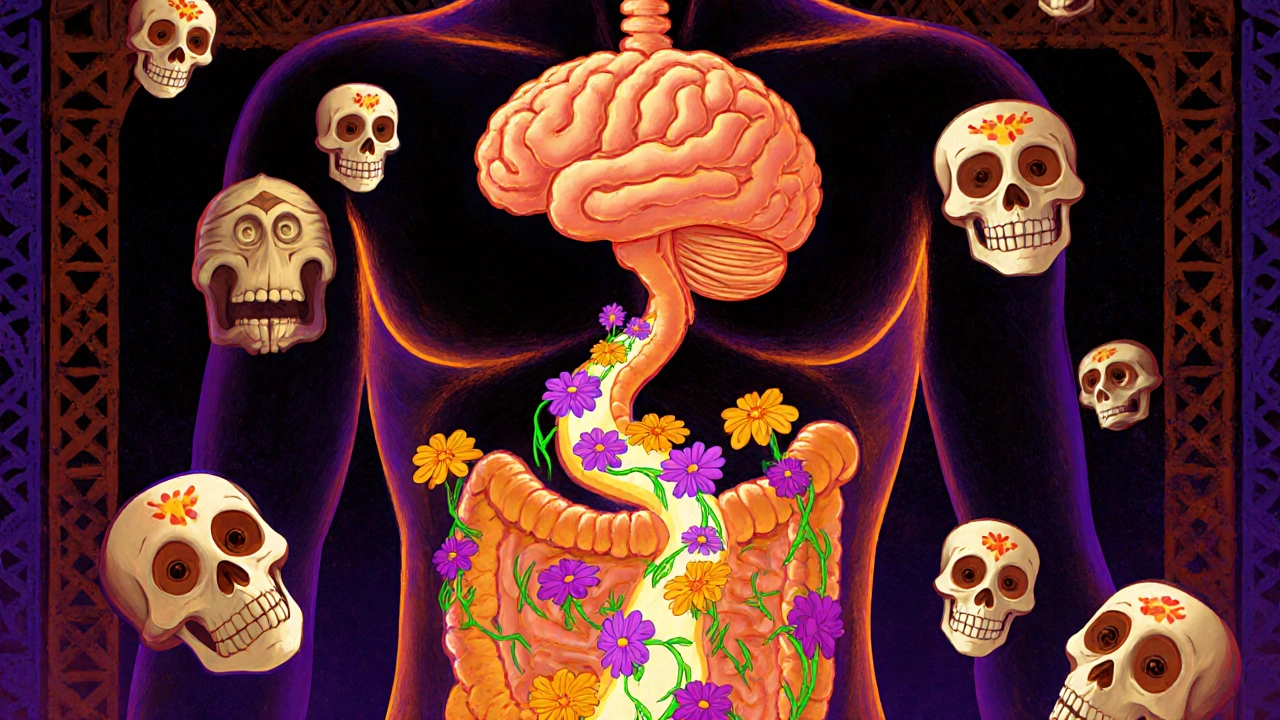
Gut-Brain Axis: How Your Digestive System Shapes Your Mood and Mental Health
When you feel nervous and get a stomachache, or feel down after eating junk food, you’re seeing the gut-brain axis, the bidirectional communication network linking your digestive tract and central nervous system. Also known as the enteric nervous system, it’s not just a metaphor—it’s a real, measurable highway of nerves, hormones, and bacteria that talks back and forth between your gut and your brain. This connection explains why stress can cause diarrhea, why antidepressants sometimes mess with your digestion, and why fixing your gut might help your anxiety.
The microbiome, the trillions of bacteria living in your intestines plays a huge role here. These tiny organisms don’t just help you digest food—they produce serotonin, dopamine, and other chemicals that directly affect your mood. Studies show people with depression often have different gut bacteria than those without. And it works both ways: if you’re chronically stressed, your gut lining can get leaky, letting in toxins that trigger inflammation—and that inflammation can make your brain feel foggy, tired, or anxious.
It’s not just about probiotics or yogurt. The digestive system, including your stomach, intestines, and liver is a major player in how your body handles medications, nutrients, and toxins. That’s why drugs like antibiotics or SSRIs can throw off your gut balance, leading to side effects that feel unrelated—like insomnia or brain fog. Even something as simple as sugar intake or artificial sweeteners can change your gut environment enough to affect your mental state, as seen in posts about acid indigestion and medication side effects.
This isn’t new-age wellness talk. It’s science backed by clinical data—like how deprescribing unnecessary meds reduces side effects and improves mental clarity, or how certain antibiotics raise potassium levels and disrupt nerve signaling. Your gut health affects everything from how you respond to anxiety meds to whether you’re prone to kidney stones from topiramate. It’s why someone on acamprosate for alcohol dependence needs counseling—their brain chemistry is tied to their gut. It’s why cystic fibrosis patients on azilsartan might see better lung function: their inflammation levels are dropping because their gut is calmer.
What you’ll find in the posts below isn’t just a list of articles. It’s a map. You’ll see how gut-brain connections show up in antibiotic use, mental health treatments, kidney stress, sleep disruption, and even how travel insurance can’t cover your gut-related flare-ups because they’re tied to long-term medication changes. This isn’t about quick fixes. It’s about understanding how your body really works—and what you can do to make it work better, from the inside out.
Irritable Bowel Syndrome is caused by a breakdown in gut-brain communication, not just digestion. Learn how diet, hypnotherapy, and new medications target the root cause for real relief.
Chris Gore Nov 10, 2025




