The Future of Contact Dermatitis Treatment: Emerging Therapies and Research

Understanding Contact Dermatitis: Causes and Symptoms
Before diving into the future of contact dermatitis treatment, it is essential to understand what contact dermatitis is and its causes. Contact dermatitis is a skin condition that occurs when an individual's skin comes into contact with a certain substance, causing irritation or an allergic reaction. Common irritants include soaps, detergents, metals, and even certain plants. In some cases, an individual's immune system may overreact to a substance, leading to an allergic response.
Symptoms of contact dermatitis can range from mild to severe and may include itching, redness, swelling, and blistering. In some cases, the affected area may become infected, leading to further complications. It is crucial to identify the cause of contact dermatitis to prevent future exposure and effectively treat the condition.
Current Treatment Options for Contact Dermatitis
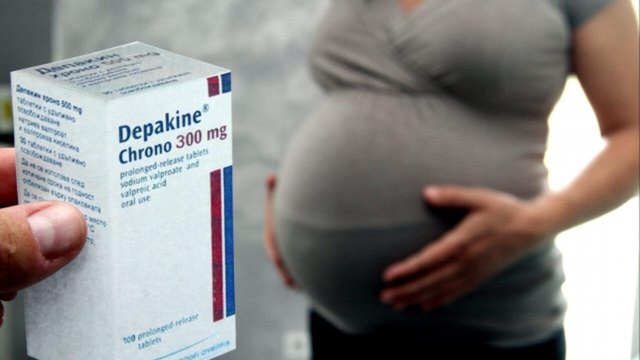
At present, the primary treatment for contact dermatitis involves avoiding the irritant or allergen causing the skin reaction. Over-the-counter creams and ointments may help alleviate symptoms, such as itching and redness. In more severe cases, prescription medications may be necessary, including corticosteroid creams, oral corticosteroids, and antihistamines.
While these treatments can be effective in managing symptoms, they may not always address the root cause of the problem. Furthermore, prolonged use of corticosteroids can lead to side effects, such as thinning of the skin, making it essential to explore alternative and more targeted treatment options.
Targeting the Immune System: Biologics and Immunotherapy
One promising area of research in contact dermatitis treatment involves targeting the immune system. Biologic drugs, which are derived from living organisms, have shown promise in treating various inflammatory skin conditions, such as psoriasis and eczema. These medications work by inhibiting specific proteins or cells involved in the inflammatory process, thereby reducing skin inflammation and irritation.
Immunotherapy is another potential treatment option for contact dermatitis. This approach involves exposing the immune system to small amounts of the allergen in a controlled manner, eventually desensitizing the body to the substance. While immunotherapy has been successful in treating other allergic conditions, such as hay fever and asthma, further research is needed to determine its effectiveness in treating contact dermatitis.
Natural Remedies and Alternative Therapies
As more people seek natural and alternative treatments for various health conditions, researchers are exploring the potential benefits of these therapies for contact dermatitis. Some studies have investigated the use of herbal remedies, such as aloe vera, calendula, and chamomile, to soothe irritated skin and reduce inflammation. While these natural treatments may provide relief for some individuals, it is essential to proceed with caution, as some herbal remedies can cause allergic reactions themselves.
Other alternative therapies being studied include acupuncture, which has shown promise in reducing itching and inflammation in some cases. However, more research is needed to determine the effectiveness of these alternative treatments for contact dermatitis.
Advancements in Topical Treatments
Topical treatments, such as creams and ointments, remain a mainstay in managing contact dermatitis symptoms. Recent advancements in this area include the development of new formulations designed to provide targeted relief with fewer side effects. For example, researchers are exploring the use of nanoparticles to deliver anti-inflammatory drugs directly to the affected skin, minimizing the risk of systemic side effects.
Additionally, new barrier creams are being developed to protect the skin from irritants and allergens more effectively, reducing the risk of contact dermatitis. These advancements in topical treatments may provide more effective and safer options for individuals suffering from this skin condition.
Gene Therapy and the Future of Contact Dermatitis Treatment
Gene therapy is an emerging area of research with the potential to revolutionize the treatment of various health conditions, including contact dermatitis. By targeting the genes responsible for causing an allergic reaction or skin irritation, researchers hope to develop treatments that can effectively cure or prevent contact dermatitis.
While gene therapy for contact dermatitis is still in its infancy, early research has shown promise. As our understanding of the genetic factors involved in this skin condition continues to grow, so too will the potential for groundbreaking treatments that address the root cause of contact dermatitis.
Personalized Medicine: Tailoring Treatments to the Individual
One of the most exciting aspects of modern medicine is the growing focus on personalized treatments. By understanding an individual's unique genetic makeup and medical history, healthcare providers can tailor treatments to provide the most effective and safest care possible. In the context of contact dermatitis, this may involve identifying specific allergens or irritants that trigger an individual's symptoms and developing targeted therapies to address these triggers.
As research continues to advance our understanding of contact dermatitis and the factors that contribute to its development, we can expect to see more personalized treatment options become available. This tailored approach to care has the potential to significantly improve the quality of life for individuals suffering from contact dermatitis.





Just a heads‑up, staying aware of any new creams on the market can make a big difference.
Honestly, the article glosses over the fact that many so‑called “advanced” biologics are just marketing tricks that end up costing patients more without delivering real benefits.
I’ve been following the recent trials on IL‑4 inhibitors, and they seem promising. Those agents target a specific cytokine pathway that drives inflammation in many dermatitis cases. The safety profile looks better than long‑term steroids, especially for people with sensitive skin. Plus, the dosing schedule is becoming more convenient, which helps adherence.
The article correctly notes “IL‑4 inhibitors” but it should be “IL‑4 inhibitors,” with a hyphen for clarity.
Another practical angle is the development of barrier creams enriched with ceramides that actually rebuild the lipid matrix of the skin. In my experience, patients who apply a ceramide‑based barrier before any exposure have fewer flare‑ups. It’s a simple step that can be combined with any of the newer topical formulations for added protection.
One must consider that the pharmaceutical industry has historically cloaked its profit motives behind the veneer of scientific progress, and the push for biologics may be no exception. The extensive marketing budgets allocate resources toward influencing prescribing habits rather than pure patient benefit. Consequently, clinicians should scrutinize the underlying data with a skeptical eye before embracing these costly interventions as panaceas.
Peering into the future of dermatitis treatment feels a bit like watching an alchemist attempt to turn lead into gold; the glitter of nanotech and gene editing tempts us with promises of miracle cures, yet we must temper our enthusiasm with the cold steel of rigorous testing. The tapestry of research is woven with threads of optimism, but every glittering strand needs the loom of evidence to hold its shape.
Sounds promising but keep an eye on long term safety.
The surge in personalized medicine is reshaping how we approach contact dermatitis, and it’s impossible not to feel the excitement buzzing through the research labs. First, genomic profiling can pinpoint specific HLA alleles that predispose individuals to allergic reactions, allowing clinicians to anticipate triggers before they manifest. Second, CRISPR‑based gene editing offers the tantalizing prospect of knocking out the very genes that amplify the inflammatory cascade, essentially rewiring the skin’s response at a molecular level. Third, the integration of wearable sensors that monitor skin pH and moisture in real time could feed data into adaptive treatment algorithms, adjusting topical potency on the fly. Fourth, the rise of biologics targeting interleukins such as IL‑13 and IL‑31 has already demonstrated reductions in itching severity, which is often the most debilitating symptom for patients. Fifth, these agents are being engineered with longer half‑lives, meaning fewer injections and better compliance. Sixth, researchers are experimenting with lipid‑based nanoparticles that can ferry anti‑inflammatory drugs directly across the stratum corneum, bypassing the barrier that usually hinders penetration. Seventh, patient registries are being compiled worldwide, providing a treasure trove of real‑world outcomes that can validate trial data. Eighth, the ethical considerations surrounding gene therapy are being addressed through community engagement and transparent consent processes, fostering trust. Ninth, insurance models are slowly adapting to cover personalized regimens, recognizing the long‑term cost savings of preventing severe flares. Tenth, interdisciplinary collaborations between dermatologists, immunologists, and bioengineers are breaking down silos, accelerating innovation. Eleventh, educational platforms are emerging to empower patients with knowledge about their own genetic risk factors, promoting proactive skin care. Twelfth, the convergence of artificial intelligence with dermatopathology is refining diagnostic accuracy, ensuring that the right therapy is matched to the right patient. Thirteenth, while enthusiasm is high, the field must remain vigilant against over‑promising, as history teaches us that every breakthrough comes with unforeseen challenges. Fourteenth, ongoing longitudinal studies will be crucial to monitor for delayed adverse effects of these cutting‑edge treatments. Fifteenth, as the science matures, we can anticipate a future where a simple skin patch could deliver a customized cocktail of therapeutics tailored to an individual’s molecular profile. Finally, the ultimate goal remains clear: to transform a condition that once caused daily discomfort into a manageable, if not negligible, aspect of life.
Agreed, the nanoparticle approach could reduce systemic exposure.
From a cultural standpoint, skin health often reflects the broader relationship between societies and their environments. When we prioritize natural barrier preservation, we acknowledge centuries of ancestral wisdom that modern medicine sometimes overlooks. Integrating that perspective with cutting‑edge science may yield the most balanced path forward.
The concept of gene therapy for dermatitis intrigues me, especially as vector delivery becomes more precise. If viral vectors can be engineered to target only the keratinocytes responsible for the allergic cascade, we might achieve lasting remission. However, scalability remains a hurdle; producing individualized viral doses for millions of patients is no small feat. Collaboration with biotech firms could streamline manufacturing pipelines, making the technology more accessible. Meanwhile, regulatory frameworks will need to evolve to keep pace with these rapid innovations.
Great insights, everyone-excited to see where this research heads.