Fludrocortisone and the Brain: An Intriguing Connection
Discovering Fludrocortisone and Its Role in the Brain
As a curious blogger, I have always been eager to explore and understand the complex world of medicine and its effect on our bodies. Recently, an intriguing connection between a synthetic steroid called Fludrocortisone and the brain caught my attention. In this article, I will delve into what Fludrocortisone is, its role in the brain, and its potential effects on various neurological conditions. So, let's embark on this fascinating journey together!
What is Fludrocortisone and How Does It Work?
Fludrocortisone is a synthetic corticosteroid hormone that is primarily used to treat conditions such as adrenal insufficiency and orthostatic hypotension. It works by mimicking the actions of aldosterone, a hormone produced by the adrenal glands, which helps regulate the balance of salt and water in the body. Fludrocortisone helps the kidneys retain sodium and eliminate potassium, leading to an increase in blood volume and blood pressure. Now that we have a basic understanding of what Fludrocortisone is, let's explore its connection to the brain.
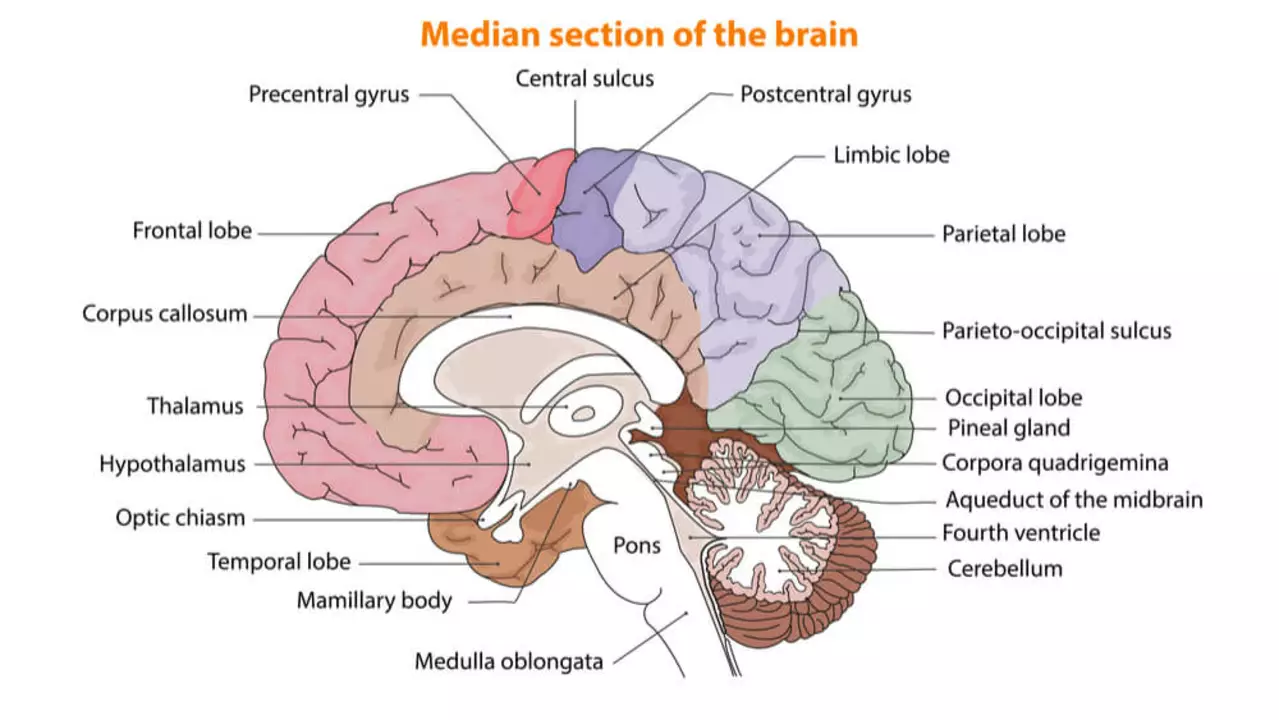
Fludrocortisone's Impact on the Blood-Brain Barrier
The blood-brain barrier is a highly selective membrane that separates the circulating blood from the brain's extracellular fluid, ensuring the brain's proper functioning. Interestingly, research has shown that Fludrocortisone can impact the integrity of the blood-brain barrier, making it more permeable. This increased permeability could potentially allow certain substances or medications to cross into the brain more easily. Consequently, the effects of Fludrocortisone on the blood-brain barrier could have significant implications on the treatment of various neurological disorders.
Neurological Disorders and Fludrocortisone
Given its effect on the blood-brain barrier, Fludrocortisone has been studied in the context of various neurological disorders, including Parkinson's disease and multiple sclerosis. Although research in this area is still ongoing, some studies have shown promising results. For instance, in Parkinson's disease, Fludrocortisone has been found to improve symptoms related to orthostatic hypotension, a common non-motor complication of the disease. Similarly, in multiple sclerosis, Fludrocortisone has been suggested as a potential treatment to help manage fatigue, one of the most debilitating symptoms of the condition.
Fludrocortisone and Its Potential Role in Treating Traumatic Brain Injuries
Another area of interest in the connection between Fludrocortisone and the brain is its potential role in treating traumatic brain injuries (TBIs). Preliminary research suggests that Fludrocortisone may help reduce brain swelling and inflammation following a TBI, which could potentially improve recovery outcomes. However, more research is needed to confirm these findings and determine the appropriate dosages and treatment protocols.
Unraveling the Mystery of Fludrocortisone's Effects on Cognition
Given Fludrocortisone's impact on the blood-brain barrier and its potential role in treating various neurological conditions, it is only natural to wonder if this synthetic steroid has any direct effects on cognition. Some studies have reported that Fludrocortisone may improve cognitive function in patients with orthostatic hypotension, while others have found no significant cognitive effects. The relationship between Fludrocortisone and cognition remains an open question, and further research is necessary to fully understand this intriguing connection.
Side Effects and Precautions When Using Fludrocortisone
As with any medication, it is important to be aware of potential side effects and precautions when using Fludrocortisone. Some common side effects include fluid retention, high blood pressure, and low potassium levels. Additionally, Fludrocortisone should be used with caution in patients with a history of heart disease, kidney disease, or high blood pressure. Always consult with your healthcare provider before starting any new medication or treatment, and be sure to discuss any potential risks or benefits associated with Fludrocortisone therapy.
Final Thoughts on Fludrocortisone and the Brain
In conclusion, Fludrocortisone is a fascinating synthetic steroid with an intriguing connection to the brain. Its impact on the blood-brain barrier and potential role in treating various neurological disorders make it a promising area for further research. As we continue to explore this connection, it is essential to stay informed and consult with healthcare professionals to ensure the safe and effective use of Fludrocortisone. I hope this article has provided you with valuable insights into the world of Fludrocortisone and its relation to the brain, and I look forward to sharing more exciting discoveries with you in the future!




Thank you for shedding light on such a niche topic. Fludrocortisone's impact on the blood‑brain barrier certainly warrants further investigation, especially given its potential to modulate drug delivery to the CNS. It would be prudent for clinicians to monitor electrolyte balance when prescribing this steroid, as the systemic effects can indirectly influence neurological health. I appreciate the thorough overview and look forward to more detailed studies on its cognitive implications.
Sounds like another excuse for the pharma lobby to push more pills.
Interesting read! While Fludrocortisone is primarily known for its mineralocorticoid activity, its ability to traverse the blood‑brain barrier-albeit modestly-opens a window for novel therapeutic avenues. In animal models, slight increases in barrier permeability have been linked to enhanced clearance of neurotoxic metabolites, which could be beneficial in diseases like Parkinson’s. However, we must tread carefully; altering barrier integrity might also permit unwanted substances to infiltrate the CNS. The orthostatic hypotension relief in Parkinson’s patients is a tangible benefit, yet the long‑term neurovascular effects remain unclear. Future trials should stratify participants by baseline BBB integrity to parse out these nuances.
Great points! It’s also worth highlighting that preserving cultural nuances in patient education can improve adherence. Explaining the steroid’s role in everyday language helps bridge the gap between complex pharmacology and patient experience. Let’s keep the conversation supportive and fact‑based.
Yo, this stuff is wild! Fludro might just be the underdog hero for TBI recovery-reducing swelling like a champ. Imagine a tiny steroid stepping in where big‑boy meds can’t get through. If we can fine‑tune the dose, we could see faster rehab times, which would be epic for patients and therapists alike. Keep the science rolling, because the more we know, the better we can fight brain trauma!
Absolutely, the potential for Fludrocortisone to aid in post‑injury inflammation is compelling. From a pharmacologic standpoint, its mineralocorticoid activity may help stabilize endothelial cells, thereby curbing edema. That said, we must balance benefits against risks like fluid overload, especially in patients with comorbid heart conditions. Ongoing dosage‑optimization studies will be key to safely harnessing these effects.
Delving into the cerebral ramifications of Fludrocortisone invites a cascade of philosophical and clinical inquiries that merit exhaustive deliberation. First, the notion that a synthetic mineralocorticoid can modulate blood‑brain barrier permeability challenges longstanding dogmas about pharmacokinetic impermeability. Second, the intersection of orthostatic hypotension management with neurocognitive outcomes raises the specter of a bidirectional feedback loop wherein systemic hemodynamics influence cerebral perfusion and vice versa. Third, the literature on Fludrocortisone’s impact on neuroinflammation is nascent but suggests an immunomodulatory capacity that could be harnessed in demyelinating diseases. Fourth, the potential for ameliorating fatigue in multiple sclerosis via electrolyte stabilization hints at a mechanistic bridge between ion homeostasis and neuronal excitability. Fifth, the ethical considerations surrounding off‑label use demand rigorous informed‑consent protocols, particularly given the specter of hypertension and hypokalemia. Sixth, the pharmacodynamic profile of Fludrocortisone, with its long half‑life, necessitates vigilant monitoring to preempt iatrogenic complications. Seventh, the role of patient‑specific factors-such as genetic polymorphisms in the mineralocorticoid receptor-may dictate therapeutic efficacy and should be a focus of precision‑medicine research. Eighth, the translational gap between rodent models showcasing reduced cerebral edema and human trials remains a formidable obstacle, underscoring the need for robust phase‑II studies. Ninth, the cognitive domain, often overlooked, may benefit from improved cerebral perfusion secondary to blood pressure stabilization, though data remain equivocal. Tenth, the interplay with concurrent therapies, such as dopamine agonists in Parkinson’s disease, raises the prospect of synergistic or antagonistic effects that must be systematically evaluated. Eleventh, the potential for Fludrocortisone to serve as a vector for delivering adjunctive neuroprotective agents across a permeabilized barrier is an intriguing avenue for drug development. Twelfth, the socioeconomic implications of prescribing a relatively inexpensive steroid versus more costly biologics could democratize access to neuroprotective strategies. Thirteenth, the necessity for multidisciplinary stewardship-entailing endocrinologists, neurologists, and pharmacists-cannot be overstated if we are to integrate Fludrocortisone into standard care pathways responsibly. Fourteenth, the longitudinal effects on renal function, given its sodium‑retaining properties, demand careful surveillance over extended treatment horizons. Fifteenth, the broader philosophical question persists: to what extent should we manipulate the blood‑brain barrier, a critical evolutionary safeguard, in pursuit of therapeutic gain? In sum, while Fludrocortisone offers a tantalizing prospect for neurologic intervention, a tapestry of clinical, ethical, and mechanistic threads must be woven together before it can be embraced as a mainstream therapeutic.
That was a powerhouse of insight. I echo the call for multidisciplinary collaboration, especially when navigating the fine line between benefit and risk. Let’s champion rigorous trials and keep patient safety front and center.
The moral dimension of meddling with our brain’s fortress cannot be ignored. While some laud the therapeutic promise, others warn that altering the blood‑brain barrier may usher in unintended consequences, akin to opening Pandora’s box. Our duty as medical custodians is to balance curiosity with caution, ensuring that the pursuit of innovation does not eclipse the sanctity of patient welfare.
I understand the concerns but also see the potential benefits. Let’s keep an open dialogue and respect each other’s viewpoints.
Patriotic physicians should prioritize home‑grown solutions like Fludrocortisone over foreign pharmaceutical monopolies.
I appreciate the passion behind your point, yet it's vital to evaluate the evidence objectively. Collaborative research can guide us toward the best outcomes for all patients.
Super excited to see where this research goes! Let’s keep sharing updates and supporting each other.