Boxed Warning Changes: How FDA Drug Safety Labels Evolve Over Time

Boxed Warning Timeline Calculator
How Long Until a Boxed Warning?
Based on FDA data showing the average 11-year delay between drug approval and boxed warning issuance
Results
The time between drug approval and boxed warning issuance was years.
The FDA's Drug Safety-related Labeling Changes (SrLC) database shows 51% of boxed warnings are issued for death risks, with 27% related to cardiovascular issues.
The boxed warning is the most serious safety alert the FDA can require on a prescription drug label. It doesn’t just sit at the bottom of a pamphlet-it’s front and center, surrounded by a thick black border, written in bold uppercase letters, and bulleted for maximum impact. This isn’t a suggestion. It’s a red flag meant to stop a prescriber in their tracks. If you’re a doctor, pharmacist, or even a patient who’s read the fine print on a medication, you’ve seen it. But what you might not realize is how often these warnings change-and how hard it is to keep up.
What Exactly Is a Boxed Warning?
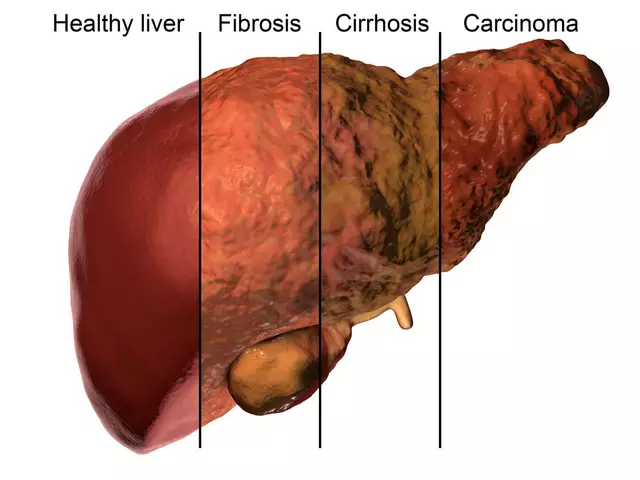
A boxed warning, sometimes called a black box warning, is the FDA’s strongest tool to warn about life-threatening risks tied to a drug. It’s not about mild side effects like nausea or dizziness. It’s about risks that can lead to death, organ failure, severe addiction, or irreversible harm. Think suicidal thoughts with antidepressants, heart attacks from diabetes drugs, or tendon rupture from antibiotics. These aren’t rare flukes-they’re patterns found after thousands of people have used the drug in real life. The format isn’t random. According to FDA regulations (21 CFR 201.57(e)), the warning must have a black border, bold header, and bullet points. It appears at the very top of the drug’s prescribing information, before even the contraindications. That placement isn’t accidental. The FDA wants it seen first. And it’s been this way since 1979, when the format was introduced to cut through the noise of dense medical labels.Why Do Boxed Warnings Change?
Most drug risks aren’t discovered in clinical trials. That’s the problem. Trials involve a few thousand people over months or a couple of years. Real-world use involves millions over decades. That’s where problems emerge. Take fluoroquinolone antibiotics, like Cipro or Levaquin. In 2008, the FDA added a boxed warning about tendon rupture after reports piled up from emergency rooms and physical therapists. By 2022, the warning was updated again to include persistent, disabling symptoms that could last for months or years-even after stopping the drug. That’s not a one-time fix. It’s an ongoing process of learning. Between 2008 and 2015, the FDA issued 111 boxed warnings. Nearly a third were brand-new. Another third were major updates-like adding new patient groups at risk or expanding the type of harm described. The rest were minor tweaks: clarifying wording, adding a monitoring recommendation, or refining the population affected. The most common triggers? Death (51% of warnings) and cardiovascular risk (27%). But the single most frequent specific concern across all drugs? Addiction. Opioids, stimulants, even some antidepressants-when the data shows a pattern of dependence or misuse, the FDA acts.How Often Are Boxed Warnings Updated?
The timeline is staggeringly slow. On average, it takes 11 years from when a drug hits the market to when the FDA issues a boxed warning. That’s up from just 7 years in the 1990s. Why? Because it takes time to gather enough real-world data. A single case of liver failure doesn’t trigger a warning. But if 50 patients across different states develop the same rare reaction, and the pattern holds up under review, then the FDA moves. Between 2008 and 2015, 64% of drugs with new boxed warnings were meant for long-term use. That makes sense-you’re more likely to see harm over years than weeks. And 58% of those drugs had safer alternatives. The FDA isn’t trying to pull drugs off the market. They’re trying to make sure the right patients get the right drugs. The FDA’s Drug Safety-related Labeling Changes (SrLC) database, launched in January 2016, is the only official public tracker for all changes since then. It’s updated weekly. But here’s the catch: before 2016, there was no central system. You had to dig through MedWatch archives, old press releases, and drug approval documents. That’s why many clinicians miss updates.Who Notices These Changes?
Surprisingly, not enough people. A 2017 FDA survey found that 87% of healthcare providers check for boxed warnings when prescribing a new drug. But 63% admitted they rarely check for updates to existing ones. Pharmacists in hospital systems often have dedicated teams. The University of Michigan, for example, spends 12 pharmacist-hours every month just reviewing new labeling changes. But in community pharmacies? Only 38% have formal monitoring systems. Most rely on automated alerts from their pharmacy software. And those alerts? 41% of pharmacists say they’re flooded with false positives-like a warning for a drug the patient isn’t even taking. On the patient side, it’s worse. Only 35% of pharmacies consistently hand out Medication Guides-the FDA-mandated patient handouts that explain risks in plain language. When they do, patient understanding jumps from 42% to 78%. But without them, patients often don’t know they’re on a drug with a boxed warning at all.What Happens When a Warning Is Added-or Removed?
The real-world impact is immediate. After the Chantix (varenicline) boxed warning for psychiatric side effects was added in 2009, prescriptions dropped by 40% in some clinics. Doctors feared lawsuits. Patients panicked. But when the FDA removed the warning in 2016-after reviewing more data-prescriptions slowly came back. Not to pre-warning levels, but close enough to show that warnings can be both overblown and corrected. The same happened with Avandia (rosiglitazone). The 2007 boxed warning for heart attack risk caused a massive drop in prescriptions. But many endocrinologists argued the data was shaky. Years later, more nuanced reviews showed the risk was real-but only for certain patients. The warning still stands, but prescribing patterns have stabilized. It’s not perfect, but it’s a conversation starter. On the flip side, fluoroquinolone warnings led to a 68% shift in prescribing habits among physicians on the Sermo forum. Internists, who often treat older patients with chronic infections, changed their approach most. Some now avoid the drugs entirely. Others use them only when no alternatives exist. That’s the goal: not to ban, but to balance.







Man i never realized how much these warnings change after the fact
My grandma was on that diabetes med that got the black box and she never even knew
She just took it cause the doctor said so
Scary stuff
11 years to add a warning? Thats not slow thats a crime
Drug companies fund the studies and the FDA gets cozy
Its not about safety its about profits
And you think theyll remove a warning when it hurts sales?
Ha
Everyone talks about the black box like its some big scary thing but the real issue is no one tells you about it
Patients deserve to know what theyre taking
Not just the doctor
Not just the pharmacist
But YOU
Ask for the guide
Its your right
And its not that hard
The current regulatory paradigm is fundamentally inadequate for the complexity of pharmacovigilance in a post-marketing surveillance context
The FDA's reliance on passive reporting systems and retrospective cohort analysis introduces significant temporal lag and selection bias
Consequently, the risk-benefit calculus is perpetually misaligned with real-world clinical outcomes
Structural reform is imperative
My doc just told me my blood pressure med got a new warning last month
I had no idea
And the app didnt even ping me
Theyre supposed to but they dont
So now i check the FDA site once a month
Its weird but its better than waiting for someone to die
Theyre hiding something
Every time they update a warning its because they knew all along
They let people get hurt to test the limits
Then they act surprised
Its all a cover for the pharmaceutical cabal
They control the FDA
They control the media
They control your mind
Why are we even letting foreign drug companies get away with this
America has the best science in the world
But we let these foreign meds come in with no real testing
Then we act shocked when people die
Its embarrassing
So many people think the black box is a death sentence
But it’s not-it’s a conversation starter
It’s a way to say: “Hey, this is serious, but it’s manageable if you’re careful”
My aunt was on Chantix, got the warning, talked to her pharmacist, switched to patches
She quit smoking and didn’t have a single panic attack
Knowledge is power-and so is asking questions
Oh wow a black box
So dramatic
Next they’ll put a skull and crossbones on my Advil
And then we’ll all have to sign a waiver to buy ibuprofen
What a world we live in
Why does everyone assume the FDA is doing the right thing
They’ve been wrong before
Remember Vioxx?
They waited years
People died
Now they’re pretending they’re heroes
They’re not
They’re bureaucrats
They don’t want you to know how much they’re guessing
Every single drug is a gamble
They test on 3000 people for 6 months
Then they release it to 50 million
And when 100 people die they call it “rare”
But 100 people is 100 families
And they still won’t change the label until someone sues them
Or a senator gets mad
Until then? You’re the lab rat
And the FDA? They’re just watching
For prescribers: the SrLC database is your best friend
Set a monthly reminder
For pharmacists: push for Medication Guides
They’re not paperwork-they’re lifelines
For patients: ask
Don’t assume
Don’t be shy
The black box isn’t there to scare you
It’s there so you can decide
And you can’t decide if you don’t know