Anaphylaxis from Medication: Emergency Response Steps You Must Know

When a medication triggers anaphylaxis, you have minutes-not hours-to act. This isn’t a slow-moving reaction. It’s a full-body emergency that can kill in under 10 minutes if ignored. And the worst part? Many people don’t recognize it until it’s too late.
What Anaphylaxis from Medication Really Looks Like
Anaphylaxis from drugs doesn’t always start with a rash or hives. In fact, up to 20% of cases show no skin symptoms at all. That’s why waiting for a visible reaction is deadly. The real warning signs are hidden in your breathing, circulation, and throat.Think about it: if someone suddenly can’t talk clearly, their voice is hoarse, or they’re gasping for air like they’re drowning on dry land-that’s not just a cold. That’s anaphylaxis. Swelling in the tongue or throat? That’s the airway closing. Dizziness, fainting, or turning pale? That’s your blood pressure crashing. These aren’t side effects. These are red flags screaming for immediate action.
Medications that cause this most often? Antibiotics like penicillin, NSAIDs like ibuprofen, contrast dyes used in scans, and muscle relaxants during surgery. But it can happen with any drug-even ones you’ve taken before without issue. Allergies don’t care about past history. One dose is all it takes.
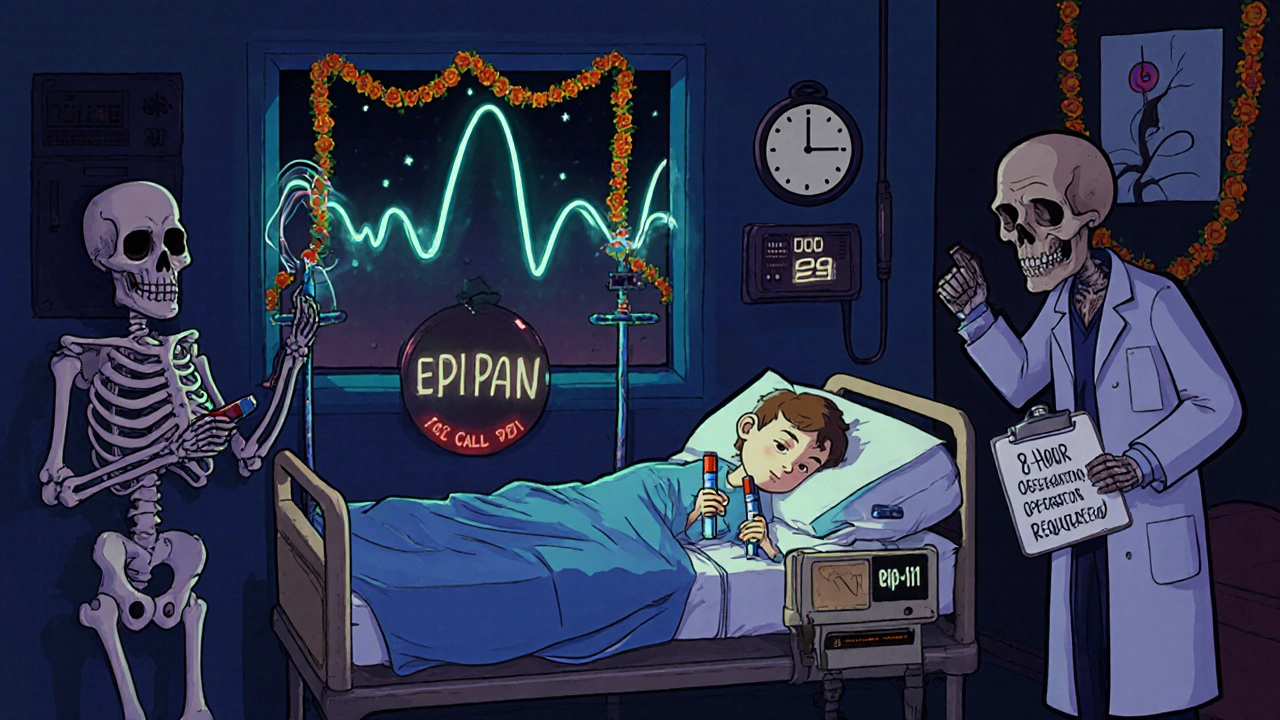
The One Thing That Saves Lives: Epinephrine
There’s only one treatment that stops anaphylaxis from killing you: epinephrine. Not antihistamines. Not steroids. Not oxygen. Not calling for help first. Epinephrine.It works in 1 to 5 minutes. It opens your airway, tightens your blood vessels, and brings your heart back from the edge. But it wears off in 10 to 20 minutes. That’s why just giving one shot isn’t enough. You need to get help immediately after.
Use the auto-injector-EpiPen, Auvi-Q, Adrenaclick-into the outer thigh. Not the arm. Not the butt. The thigh. Muscle. That’s where it absorbs fastest. For adults and kids over 30 kg, use 0.3 mg. For kids 15-30 kg, use 0.15 mg. If you’re unsure, give it anyway. The risk of not giving it is death. The risk of giving it? A racing heart for a few minutes. That’s it.
Studies show 70% of people who die from anaphylaxis never got epinephrine. Not because they didn’t have it. Because they were afraid to use it. Or they waited to see if it got worse. Don’t be one of them. If in doubt, give it.
Positioning: Don’t Let Them Stand Up
This is where most people mess up. When someone’s having anaphylaxis, you must lay them flat. Immediately. No standing. No sitting up. No walking to the car.Why? Because standing or even sitting upright can cause sudden cardiovascular collapse in 15-20% of cases. Your blood pressure drops fast. Gravity pulls blood away from your brain and heart. Lying flat keeps blood flowing where it’s needed.
If they’re unconscious, roll them onto their left side-especially if they’re pregnant. That’s the recovery position. It keeps the airway open and prevents choking. If they’re having trouble breathing, let them sit up with legs stretched out. But don’t let them move around. Hold young children flat on their back. Never hold them upright.
Real-world data from Australia shows 55% of bystanders let patients stand during reactions. That’s not just wrong-it’s deadly. You’re not helping by trying to be helpful. You’re making it worse.

Call Emergency Services-Right After the Shot
Don’t wait. Don’t text. Don’t call a friend. Call 911 (or your local emergency number) the moment you give epinephrine. Even if they seem better.Why? Because anaphylaxis can come back. In 20% of cases, a second wave hits 1 to 72 hours later. That’s called a biphasic reaction. And it’s just as dangerous as the first. Hospitals need to monitor patients for at least 4 hours. Some guidelines now say 6-8 hours for drug-induced cases, since they carry a 25% higher risk than food-triggered ones.
Emergency crews will give IV fluids, oxygen, and possibly a second dose of epinephrine if needed. They’ll also check for other issues like asthma attacks or heart problems that can mimic anaphylaxis. But none of that matters if you didn’t give the first shot on time.
What NOT to Do
Let’s clear up the myths:- Don’t give antihistamines like Benadryl first. They help with itching or hives-but they do nothing for breathing or blood pressure. Relying on them delays real treatment. In fact, studies show zero improvement in survival rates when used alone.
- Don’t give steroids. Hydrocortisone or prednisone won’t stop the reaction. They’re sometimes used to prevent biphasic reactions, but they’re not first-line. Don’t waste time on them.
- Don’t wait for a doctor’s order. In hospitals, staff often delay epinephrine because they’re waiting for confirmation. That’s dangerous. The Resuscitation Council UK says: if symptoms point to anaphylaxis, give epinephrine. No waiting.
- Don’t inject into fat. If you miss the muscle, the drug won’t absorb fast enough. Pinch the thigh and inject into the firm part, not the soft part.
- Don’t remove the auto-injector too soon. Hold it in place for 10 seconds. That’s how long it takes to deliver the full dose. Most people pull it out after 3 seconds. That’s not enough.
Why People Delay-And How to Beat It
In hospitals, the average time from symptom recognition to epinephrine is over 8 minutes. That’s 3 minutes too long. Why? Nurses and doctors fear side effects-racing heart, high blood pressure. But here’s the truth: out of 35,000 epinephrine doses given for anaphylaxis, only 0.03% caused serious heart problems. The rest? Safe. Effective. Life-saving.In homes, 68% of people with known allergies carry an auto-injector. But only 41% feel confident using it. That’s terrifying. You can have the best tool in the world and still let someone die because you froze.
Practice. Every time you refill your prescription, take 2 minutes to practice on a training device. Watch a video. Do it with a family member. Make it routine. The more you do it, the less scary it feels.
And if you’re caring for someone with a known drug allergy? Make sure they have two auto-injectors. Always. One can fail. One can be left at home. Two is the minimum.
What’s New in 2025
The FDA approved a new auto-injector in 2023 with voice guidance-Auvi-Q 4.0. It talks you through each step. “Press firmly against thigh.” “Hold for 10 seconds.” “Call 911.” In trials, untrained users got it right 89% of the time-up from 63%. That’s huge.Research is also shifting how we dose epinephrine. Instead of just weight, doctors are starting to look at body mass index (BMI). Obese patients (BMI over 30) often need higher doses to get the same effect. Early data shows using BMI-based dosing improves blood levels by 18%.
And hospitals are starting to require 6-8 hours of observation for drug-induced cases, not just 4. Why? Because the risk of a second reaction is higher. Don’t leave early just because they seem okay.
Final Reminder: Speed Saves Lives
Anaphylaxis from medication is rare-but deadly. And the difference between life and death isn’t the drug. It’s the response.You don’t need to be a doctor. You don’t need to know the exact cause. You just need to know this:
- Recognize the signs-breathing trouble, throat swelling, dizziness.
- Give epinephrine into the thigh-right away.
- Lay them flat.
- Call emergency services.
- Stay with them. Be ready to give a second shot if symptoms return.
There’s no time for hesitation. No time for doubt. No time to Google it. If you see it, treat it. Epinephrine first. Always.
Can anaphylaxis happen the first time someone takes a medication?
Yes. Anaphylaxis doesn’t require prior exposure. The immune system can become sensitized after one dose, even if there were no previous reactions. This is why sudden, severe reactions can occur with drugs you’ve taken before without issue.
Can I use an expired epinephrine auto-injector?
If it’s your only option, yes-use it. While potency decreases over time, studies show even expired epinephrine still contains enough active drug to be life-saving. Don’t wait for a replacement. Use it, then get a new one immediately.
Why can’t I just give a Benadryl shot instead of epinephrine?
Benadryl only treats mild skin symptoms like itching or hives. It does nothing to stop airway swelling, low blood pressure, or shock-the real killers in anaphylaxis. Relying on it delays life-saving treatment and increases death risk.
What if I’m not sure it’s anaphylaxis?
If symptoms include breathing trouble, throat tightness, dizziness, or collapse-give epinephrine. The guidelines say: IF IN DOUBT, GIVE ADRENALINE. The risk of giving it unnecessarily is far lower than the risk of not giving it when it’s needed.
Do I need to go to the hospital even if I feel fine after the shot?
Yes. Even if symptoms disappear, a second reaction (biphasic anaphylaxis) can happen hours later. Hospitals must monitor you for at least 4 hours, and up to 8 hours for drug-induced cases. Leaving early could be fatal.
Can beta-blockers make anaphylaxis worse?
Yes. Beta-blockers, commonly used for high blood pressure or heart conditions, can make epinephrine less effective. Patients on these drugs may need higher doses of epinephrine and are at greater risk of severe reactions. Always tell medical staff if you’re taking beta-blockers.







Why are we letting the government force epinephrine down everyone's throat? My cousin took penicillin 10 times and never had a problem. Now they want us to carry needles like we're in a war zone. This is fearmongering.
Oh wow, another ‘epinephrine first’ lecture. Because nothing says American superiority like turning every medical emergency into a Hollywood action scene. Next they’ll make us wear EpiPens as necklaces. 🇺🇸
My sister had a reaction to ibuprofen last year - no hives, just her voice went weird and she couldn’t breathe. We didn’t know what was happening until her friend yelled, ‘GIVE HER THE PEN!’ We had one in the car. She’s alive today because we didn’t wait. This post? It’s a gift. Thank you for saying it plainly.
It’s wild how we treat medical emergencies like moral tests. We panic over a missed deadline but freeze when someone’s throat is closing. Epinephrine isn’t a weapon - it’s a bridge between panic and survival. 🙏
And yeah, I’ve practiced on my training pen with my kids. It’s like fire drills. You don’t wait for the flames to start.
This is so helpful. I’ve been scared to use my EpiPen because I didn’t want to ‘overreact.’ Now I know - better to overreact than underreact. I’m keeping two in my purse from now on. 💕
If you don’t have an EpiPen, you’re irresponsible. If you wait for a rash, you’re a danger. If you use Benadryl first, you’re killing someone slowly. This isn’t advice - it’s a survival checklist. Stop being lazy.
Bro, in India we don’t even have EpiPens in most towns. We use ice packs and pray. This post is nice but… it’s like telling someone without shoes to run a marathon. 😅
Wait - I just checked my EpiPen… it expired last month. I’m gonna go get a new one right now. Also, I didn’t know you had to hold it for 10 seconds - I’ve been doing 3. Yikes. Thanks for the wake-up call.
Epinephrine is a Big Pharma scam. The real cause of anaphylaxis? 5G signals messing with your immune system. They want you scared so you buy their needles. And the ‘biphasic reaction’? That’s just the government tracking you through your EpiPen. 🕵️♀️