Peripheral Neuropathy: Causes, Symptoms, and Medication Management
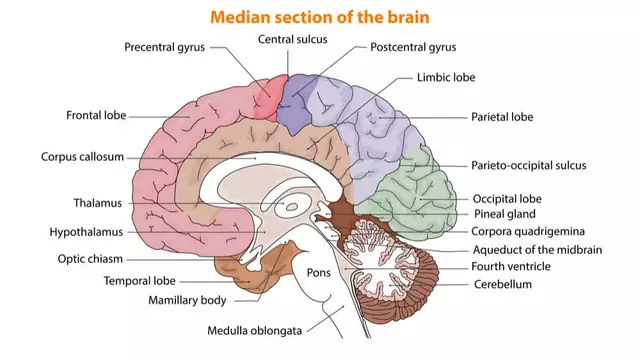
When your peripheral neuropathy, a condition where nerves outside the brain and spinal cord get damaged, leading to pain, tingling, or weakness in the limbs. Also known as nerve damage, it often starts quietly—a tingling in the toes, a burning sensation in the feet—and creeps up until daily tasks become a struggle. It’s not just aging. Diabetes is the biggest culprit, but it’s also triggered by chemotherapy, long-term alcohol use, vitamin deficiencies, and even some common prescriptions like antibiotics or blood pressure meds.
People with diabetic neuropathy, nerve damage caused by high blood sugar over time often feel it first in their feet. But medication side effects, unintended nerve damage from drugs like trimethoprim, topiramate, or certain antidepressants are a growing concern. Some meds that help one problem—like high blood pressure or depression—can accidentally hurt your nerves. That’s why knowing your meds is just as important as knowing your symptoms.
It’s not just about painkillers. Managing peripheral neuropathy means looking at the whole picture: blood sugar control, vitamin B12 levels, avoiding alcohol, and checking if any of your daily pills might be making things worse. Some people find relief with physical therapy, others with nerve-targeted meds, and some just need to switch one drug for another. The key is catching it early—before the numbness turns into falls, burns, or infections you don’t feel until it’s too late.
Below, you’ll find real-world guides on how to spot nerve damage from common meds, how to talk to your doctor about alternatives, and what treatments actually work without adding more pills to your routine. No fluff. Just what you need to protect your nerves and keep moving.
Amiodarone can cause peripheral neuropathy - numbness, tingling, and pain in hands and feet - especially after long-term use. Learn the risks, signs, and safer alternatives.
Chris Gore Nov 18, 2025