QT Prolongation Monitoring: Managing Fluoroquinolone and Macrolide Risks
QT Prolongation Risk Assessment Tool
QT Prolongation Calculator
Calculate corrected QT interval using the standard Fridericia formula (recommended) and compare with Bazett's formula.
QT prolongation is a cardiac electrophysiological abnormality characterized by delayed ventricular repolarization that can lead to potentially fatal ventricular arrhythmias, particularly Torsades de Pointes (TdP). This isn't just a lab curiosity-it's a ticking time bomb. When certain antibiotics like fluoroquinolones and macrolides disrupt the heart's electrical rhythm, the result can be fatal arrhythmias. Every year, hundreds of patients develop life-threatening heart rhythms from common antibiotics.
What QT Prolongation Really Is and Why It Matters
Here's the core mechanism: these drugs block the hERG potassium channel (IKr), which slows down the heart's repolarization phase. When this happens, the QT interval on an ECG stretches. If it gets too long, the heart can develop TdP-a dangerous arrhythmia that often leads to sudden cardiac death. The FDA has issued multiple warnings about this risk, especially for fluoroquinolones like moxifloxacin and macrolides like erythromycin.
Which Antibiotics Carry the Highest Risk?
Not all fluoroquinolones and macrolides are created equal when it comes to QT prolongation. Knowing the differences can help you choose safer options for your patients.
For fluoroquinolones:
- Moxifloxacin: Highest risk among commonly used fluoroquinolones. Studies show it can increase QTc by 10-15 ms on average.
- Levofloxacin: Moderate risk. While safer than moxifloxacin, it still poses significant risk in vulnerable patients.
- Ciprofloxacin: Lowest risk among fluoroquinolones. Often considered a safer alternative for patients with cardiac concerns.
For macrolides:
- Erythromycin: Highest risk. Known to prolong QTc significantly, especially when given intravenously.
- Clarithromycin: Moderate risk. Less than erythromycin but still concerning.
- Azithromycin: Lowest risk among macrolides. Often recommended as a safer alternative when possible.
The British Thoracic Society guidelines (2023) clearly state that erythromycin and moxifloxacin should be avoided in patients with multiple risk factors for QT prolongation. Instead, they recommend azithromycin or ciprofloxacin when appropriate.
How to Measure QT Correctly (Forget Bazett's Formula)
Measuring QT prolongation isn't as simple as reading an ECG. Many clinicians still use Bazett's formula (QTc = QT/√RR), but this method is outdated and inaccurate. The Fridericia formula (QTc = QT/√RR³) is now the gold standard because it corrects better for heart rate changes.
Here's why it matters:
- Bazett's formula overcorrects at high heart rates and undercorrects at low heart rates. This can lead to false negatives or positives.
- Fridericia's formula has been shown to better predict 30-day and 1-year mortality in patients with QT prolongation.
- Clinical guidelines now explicitly recommend Fridericia for QTc correction in all settings.
For example, a patient with a QT interval of 450 ms and RR interval of 800 ms (heart rate 75 bpm) would have:
- Bazett's QTc: 450 / √0.8 = 503 ms
- Fridericia's QTc: 450 / √(0.8³) = 473 ms
That 30 ms difference could mean the difference between a "normal" reading and a dangerous one. Always use Fridericia for accurate assessment.

Step-by-Step Monitoring Protocol
Monitoring isn't optional-it's critical. Here's exactly how to do it right:
For macrolides:
- Before starting: Get a baseline ECG to check QTc. British Thoracic Society guidelines state QTc >450 ms for men or >470 ms for women requires caution.
- One month after starting: Repeat ECG to check for new prolongation. If QTc increases by >60 ms from baseline or exceeds 500 ms, stop the drug immediately.
For fluoroquinolones:
- 7-15 days after starting: First ECG check. This is when QT prolongation typically peaks.
- Monthly for the first 3 months: Regular monitoring during this high-risk period.
- After 3 months: Periodic checks (e.g., every 3-6 months) if continuing therapy long-term.
The VUMC Antimicrobial Stewardship Program adds a key detail: "ECG monitoring should occur preferably 2 hours after administration of the antimicrobial." This timing captures peak drug effect. For patients with no risk factors and no history of prolonged QTc, monitoring isn't necessary unless new risks emerge.
Key Risk Factors That Amplify Danger
QT prolongation risk isn't just about the drug-it's about the patient. These factors multiply the danger:
- Age and gender: Women over 65 have 2-3 times higher risk of TdP. Older adults generally have higher risk.
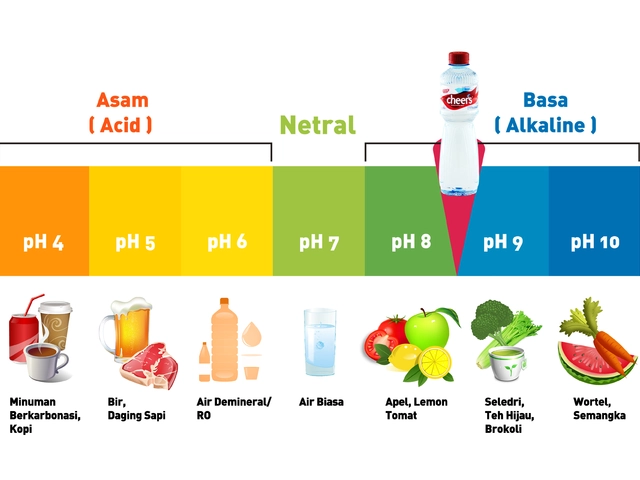
- Electrolyte imbalances: Potassium below 3.5 mmol/L or magnesium below 1.7 mg/dL dramatically increase risk.
- Other QT-prolonging drugs: Combining fluoroquinolones or macrolides with drugs like amiodarone or antiarrhythmics is extremely dangerous.
- Heart conditions: Left ventricular hypertrophy, ejection fraction below 40%, or ischemic heart disease.
- Renal or liver impairment: These can cause drug accumulation, increasing QT effects.
For example, a 72-year-old woman on ciprofloxacin for a UTI who also takes a diuretic and has low potassium is at high risk. The British Thoracic Society specifically warns against fluoroquinolone use for uncomplicated UTIs in older women with multiple comorbidities.

What to Do When QT Prolongation Occurs
Here's the critical action plan:
- Stop the antibiotic immediately if QTc exceeds 500 ms or increases by >60 ms from baseline.
- Correct electrolytes: Target potassium >4.0 mmol/L and magnesium >2.0 mg/dL. This often reverses the prolongation.
- Consider alternatives: Switch to a lower-risk antibiotic like azithromycin or ciprofloxacin (for fluoroquinolone-induced cases).
- Continuous telemetry: For patients with significant prolongation or TdP, monitor continuously until stable.
A 2021 study by FA Berger et al. documented that in ICU patients, continuous ECG monitoring every 30 seconds detected QTc changes early, allowing timely intervention. This is especially crucial in critically ill patients who often have multiple overlapping risk factors.
Real-World Case Example
Let's look at a real case: A 78-year-old woman with a history of diabetes and hypertension was prescribed levofloxacin for a urinary tract infection. She was also taking a diuretic that lowered her potassium to 3.2 mmol/L. Her baseline ECG showed QTc of 430 ms (Fridericia). Ten days later, her repeat ECG showed QTc of 510 ms. The team stopped levofloxacin immediately, replaced potassium, and switched to azithromycin. Within 24 hours, her QTc returned to normal at 440 ms. This case perfectly illustrates why monitoring and risk factor management matter.
How often should I check ECG for patients on fluoroquinolones?
For fluoroquinolones, the first ECG should be done 7-15 days after starting treatment. Then, monitor monthly for the first three months. After that, periodic checks (every 3-6 months) are recommended if therapy continues long-term. Always check ECG 2 hours after drug administration for peak effect.
Is azithromycin safer than erythromycin for QT prolongation?
Yes, azithromycin has a significantly lower risk of QT prolongation compared to erythromycin. Erythromycin strongly inhibits the hERG channel, while azithromycin has minimal effect. Clinical guidelines now recommend azithromycin as the preferred macrolide for patients with cardiac risk factors.
Can I use ciprofloxacin instead of moxifloxacin to reduce risk?
Absolutely. Ciprofloxacin carries the lowest QT prolongation risk among fluoroquinolones. The FDA and VUMC guidelines specifically recommend ciprofloxacin over moxifloxacin for patients with cardiac risk factors or when QT monitoring isn't feasible.
What's the threshold for stopping an antibiotic due to QT prolongation?
Stop immediately if QTc exceeds 500 ms or increases by more than 60 ms from baseline. This is the standard threshold in current guidelines, including those from the British Thoracic Society and FDA warnings. Also, discontinue if the patient develops symptoms like dizziness or palpitations.
Why is Fridericia formula better than Bazett's for QT correction?
Bazett's formula overcorrects at high heart rates and undercorrects at low heart rates, leading to inaccurate QTc values. Fridericia's formula (QTc = QT/√RR³) provides more accurate correction and better predicts mortality risk. It's now the recommended method in all major guidelines, including the 2023 British Thoracic Society guidelines.




Always check electrolytes.
QT prolongation is a complex interplay of drug effects and patient factors. Understanding the nuances can save lives. Always consider individual risk profiles. 🌱
The hERG potassium channel blockade by fluoroquinolones and macrolides necessitates meticulous QTc monitoring. Utilizing Fridericia correction is essential for accurate assessment. Collaboration among healthcare providers is key to mitigating risks.
Oh great, another 'life-threatening' antibiotic. Sure, let's just avoid all antibiotics and let infections run rampant. 🙄
Omg these antibiotics are so dang dangerous. Like moxifloxacin can cause TdP. People dying left right. No one checks QTc. 😭
Let's work together to improve QT monitoring! Small changes in practice can make a huge difference. Always check electrolytes and use Fridericia formula. 💪
Using azithromycin over erythromycin is basic knowledge. If you don't know this, you shouldn't be prescribing. Always use Fridericia formula.
Seriously, these antibiotics are so risky. I've seen so many cases. It's scary. People don't take this seriously. 😭
Most clinicians are clueless. They don't even know Fridericia formula. It's all Bazett's nonsense. Only experts like me know the real deal. 😒
It is imperative that clinicians adhere strictly to the British Thoracic Society guidelines. Failure to do so constitutes negligence. Patients' lives are at stake. No shortcuts.
Big Pharma manipulates drug warnings. FDA only addresses moxifloxacin to hide macrolide dangers. It's all a scam. 💀
I just can't believe how many patients are at risk...
The hERG channel blockage is so dangerous...
We need to monitor more closely...
It's terrifying...
Every single case... 😢
Moxifloxacin and low potassium dangerous combo. QTc jumps fast. Always check electrolytes 🌟