Hormone Therapy for Breast Cancer: Tamoxifen vs Aromatase Inhibitors Explained

When you’re diagnosed with hormone receptor-positive breast cancer, your doctor will likely mention hormone therapy. It’s not chemotherapy. It doesn’t make you lose your hair. But it can be just as life-changing - and sometimes harder to stick with. Two drugs dominate this space: tamoxifen and aromatase inhibitors. They work differently, have different side effects, and aren’t right for everyone. Knowing which one fits your body, your life, and your risks isn’t just helpful - it’s essential.
How Hormone Therapy Stops Breast Cancer From Coming Back
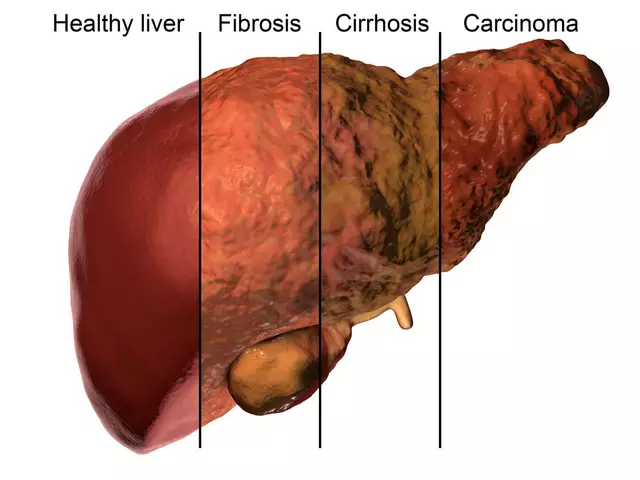
Breast cancer doesn’t grow the same way in every person. About 8 out of 10 cases are fueled by estrogen. That’s the key. If you can block estrogen from reaching cancer cells, you can stop them from growing. That’s the whole idea behind hormone therapy. It doesn’t kill cancer. It starves it. Tamoxifen and aromatase inhibitors both do this - but in completely different ways. Tamoxifen acts like a fake key. It slips into the estrogen lock on cancer cells and blocks the real estrogen from getting in. Aromatase inhibitors are more like a factory shutdown. They stop your body from making estrogen in the first place. This difference matters because your body makes estrogen differently depending on whether you’ve gone through menopause. Before menopause, your ovaries are the main source. After menopause, fat tissue and other organs take over using an enzyme called aromatase. That’s why the choice between these two drugs isn’t just about preference - it’s about biology.Tamoxifen: The Long-Standing Choice
Tamoxifen has been around since the 1970s. It was the first drug proven to cut breast cancer recurrence by half in early trials. Even today, it’s the go-to for premenopausal women. Why? Because aromatase inhibitors don’t work well if your ovaries are still producing estrogen. Tamoxifen does. It’s taken as a pill once a day, usually for 5 to 10 years. The dose is simple: 20 mg. It stays active in your system for days after you miss a pill, so occasional forgetfulness isn’t a disaster. But it’s not without trade-offs. The biggest concern with tamoxifen is its effect on the uterus. It can cause the lining to thicken, raising the risk of endometrial cancer. About 1 in 100 women on tamoxifen for 10 years will develop it - compared to 4 in 1,000 on aromatase inhibitors. That’s why annual pelvic exams are recommended. It also increases the risk of blood clots and stroke. If you’ve had a clot before, or you’re a smoker, or you’re overweight, your doctor will weigh this carefully. But tamoxifen has a silver lining: it protects your bones. Unlike aromatase inhibitors, it doesn’t make them weaker. For younger women, that’s a big deal.Aromatase Inhibitors: The New Standard for Postmenopausal Women
Aromatase inhibitors - anastrozole, letrozole, exemestane - came later. They’re not magic, but they’re more effective than tamoxifen for women who no longer have functioning ovaries. The data is clear: for postmenopausal women, AIs reduce the chance of cancer coming back by about 30% compared to tamoxifen over 5 years. These drugs slash estrogen levels by 95% or more. In postmenopausal women, estrogen isn’t coming from the ovaries anymore - it’s made in fat, muscle, and other tissues. Aromatase inhibitors block the enzyme that turns male hormones into estrogen. That’s why they only work after menopause. The catch? They strip your body of estrogen completely. That’s great for stopping cancer, but terrible for your joints, your bones, and your heart. About half of women on AIs report joint pain - sometimes so bad they can’t lift a coffee cup. It’s not just discomfort; it’s a reason many stop treatment. Studies show 22% of AI users quit because of it, compared to 8% on tamoxifen. Bone density drops fast. After 5 years on an AI, the fracture risk jumps from 5% to over 7%. That’s why doctors start DEXA scans early - usually within the first year. If your bone score falls below -2.0, you’ll likely be put on a drug like zoledronic acid or denosumab to protect your skeleton. You also might feel more tired. Some women say their brain fog gets worse. Hot flashes? They still happen - but less than with tamoxifen.
What If You’re Still Having Periods?
This is where things get complicated. If you’re premenopausal and your cancer is hormone-sensitive, you can’t just take an aromatase inhibitor. Your ovaries will keep making estrogen, and the drug won’t work. But there’s a solution: ovarian function suppression (OFS). This means either taking a monthly shot (like goserelin) or having your ovaries removed. Once your ovaries are turned off, you become postmenopausal - and then you can safely use an AI. The TEXT and SOFT trials showed that for women with higher-risk cancer, combining an AI with OFS cuts recurrence risk by 21% compared to tamoxifen alone. That sounds small - a 3.2% absolute reduction - but it means one extra woman out of every 31 avoids a recurrence. Still, not everyone needs this. If your cancer is low-risk, tamoxifen alone is often enough. It’s less intense, less expensive, and easier to live with. The decision isn’t just medical - it’s personal.Side Effects: What Real Women Are Saying
Numbers tell part of the story. Real lives tell the rest. On online forums, women on aromatase inhibitors talk about stiffness in their fingers, walking like they’re 80, and canceling weekend hikes because their knees hurt. One woman wrote: “I thought the cancer was the hard part. Turns out, the pill is what broke me.” Tamoxifen users talk about hot flashes that hit like a furnace - waking them up at 3 a.m., drenching their sheets. Some say their mood swings are worse than during puberty. But they also say: “At least I can still carry my grandkids.” A 2022 study from MD Anderson found that 64% of women would choose the same treatment again. But the reasons were different. AI users chose it because they didn’t want cancer back. Tamoxifen users chose it because they didn’t want to lose their mobility. It’s not about which drug is “better.” It’s about which side effects you’re willing to live with.How Long Do You Take It?
Five years used to be the standard. Now, we know longer is better - for some. For average-risk women, 5 years is enough. For those with higher risk - larger tumors, positive lymph nodes, aggressive grades - 7 to 10 years is recommended. The MA.17X trial showed that extending AI therapy to 10 years reduced late recurrences even further. But here’s the twist: you don’t always have to start with the best drug. Some women start with tamoxifen for 2-3 years, then switch to an AI. The OBSERVATION registry found this approach works just as well as starting with an AI. That’s good news if you can’t tolerate the side effects right away.
Cost, Access, and Global Reality
In Australia, the U.S., or the U.K., AIs are covered by insurance. But they cost up to $150 a month. Tamoxifen? Generic tamoxifen is $15 a month. That’s not just a price difference - it’s a life-or-death gap. In low-income countries, tamoxifen is often the only option. And it’s still effective. The World Health Organization lists it as an essential medicine for a reason. Even in wealthy nations, not everyone can afford copays or time off for bone scans. That’s part of the decision too. Treatment isn’t just about science - it’s about sustainability.What’s Next? New Drugs on the Horizon
The field isn’t standing still. In 2023, the FDA approved camizestrant, a new oral drug that destroys estrogen receptors instead of just blocking them. Early results show it’s more effective than AIs in tumors with certain mutations. There’s also ongoing research into genetic testing. Some people metabolize tamoxifen poorly because of their CYP2D6 gene. If you’re one of them, tamoxifen might not work well - even if you take it perfectly. Trials are now testing whether we should test for this before prescribing. And the PERSEPHONE trial is asking: Do we really need 5 years of tamoxifen? Maybe 3 is enough for low-risk cases. If so, that could spare thousands of women from unnecessary side effects.How Do You Decide?
There’s no single right answer. Your doctor will look at your age, menopausal status, cancer stage, tumor grade, and genetic markers like Oncotype DX. But the final choice? That’s yours. Ask yourself:- What side effects scare you the most? Blood clots? Joint pain? Uterine bleeding?
- How important is preserving your bone health right now?
- Can you manage monthly injections if OFS is needed?
- Will you be able to stick with daily pills for 5-10 years?
Is tamoxifen still used today?
Yes. Tamoxifen remains the standard first-line hormone therapy for premenopausal women with hormone receptor-positive breast cancer. It’s also used in men with breast cancer and in some postmenopausal women who can’t tolerate aromatase inhibitors. Its ability to protect bone density and its low cost make it a vital option, even with newer drugs available.
Can you switch from tamoxifen to an aromatase inhibitor?
Absolutely. Many women start with tamoxifen for 2-3 years, then switch to an aromatase inhibitor for the remaining 2-7 years. This approach, called sequential therapy, is just as effective as starting with an AI from day one - and often easier to tolerate. The switch is typically made after menopause occurs or when side effects from tamoxifen become too difficult.
Why don’t aromatase inhibitors work for premenopausal women?
Aromatase inhibitors block estrogen made in fat and other tissues, but they don’t stop the ovaries from producing estrogen. In premenopausal women, the ovaries are still active and pump out large amounts of estrogen - far more than the aromatase enzyme can produce. So unless ovarian function is suppressed with drugs or surgery, AIs won’t lower estrogen enough to stop cancer growth.
Do aromatase inhibitors cause weight gain?
Weight gain isn’t directly caused by aromatase inhibitors, but it’s common among users. This is likely due to a combination of factors: reduced physical activity from joint pain, changes in metabolism from low estrogen, and the natural aging process. Many women gain 2-5 kg over 5 years on AIs - not because the drug makes them fat, but because it makes movement harder and metabolism slower.
How do you know if hormone therapy is working?
Hormone therapy doesn’t shrink tumors like chemotherapy. Its job is to prevent recurrence. There’s no blood test or scan that shows it’s working. Instead, doctors track outcomes over years: if your cancer hasn’t returned after 5 or 10 years, the therapy is doing its job. Regular check-ups, mammograms, and bone scans are how you monitor your health - not the drug’s direct effect.





My mom did tamoxifen for 7 years. She said the hot flashes were brutal, but she never lost her balance or her ability to dance with her grandkids. That’s worth it to her. I wish more doctors talked about quality of life, not just recurrence stats.
The data presented here is clinically accurate and aligns with current NCCN guidelines. Hormone therapy selection must be individualized based on menopausal status, risk profile, and patient preference. Long-term adherence remains a critical factor in outcomes.
okay so i just read this whole thing and im crying. not because im scared but because i finally get it. i thought it was just ‘take a pill and hope’ but nooo it’s like choosing which version of your future self you wanna be. the one who walks without pain or the one who doesn’t wake up to cancer again. i’m gonna talk to my oncologist tomorrow. thank you.
For premenopausal women considering OFS + AI, it’s worth noting that the added benefit is most pronounced in those with node-positive or high genomic risk disease. For low-risk cases, tamoxifen alone remains a perfectly valid choice. Avoid over-treatment.
Let me just say this - I’ve seen women on AIs who can’t even hold a coffee cup because their hands are stiff, and then I’ve seen women on tamoxifen who are so tired of hot flashes they sleep in the bathtub just to cool down. Neither option is easy. But here’s the thing: the fact that we even have choices? That’s progress. We used to get one drug and pray. Now we get to pick our suffering. And that’s kind of beautiful in a messed-up way. Also, if you’re thinking about switching from tamoxifen to an AI after a few years? Do it. It’s not failure. It’s strategy.
The philosophical underpinning of hormone therapy lies not in the pharmacodynamics of estrogen blockade, but in the existential negotiation between longevity and lived experience. One must ask: is survival without vitality, survival at all?
Important note: the 22% discontinuation rate for joint pain with AIs is from the ABCSG-12 trial - but many women don’t realize that physical therapy, low-impact exercise, and even vitamin D3 can help reduce it significantly. Also, if you’re on an AI and your bone density is dropping, ask about denosumab - it’s not just for osteoporosis, it’s a cancer survival tool too. And yes, tamoxifen can cause mood swings - but SSRIs like sertraline often help without interfering with its efficacy. Talk to your care team - don’t just quit.
Man, I read this like a novel. In India, tamoxifen is the only thing we have - and it’s like gold dust. My aunt took it for 10 years, no problems, just hot flashes and a lot of chai. But I know women in Mumbai who can’t even afford the bus ride to the hospital for scans. This isn’t just medicine - it’s justice. If you’re lucky enough to have options, don’t take them for granted. Someone else is praying for a $15 pill.
So let me get this straight - we’re telling women to pick between uterine cancer and being unable to hold a spoon? That’s not treatment, that’s torture wrapped in a clinical trial. And why are we still pushing 10 years? Who even lives that long after cancer? Just give me the chemo and let me get on with my life.
My sister switched from tamoxifen to letrozole after 3 years. Said her joints hurt less than her hot flashes. Also, she started yoga. Weirdly, it helped. Just saying - you don’t have to suffer in silence. There are ways to cope. Talk to other survivors. Reddit’s got a whole army of them.
Every choice here is a quiet act of courage. Not the loud kind - the kind where you wake up at 3 a.m. drenched in sweat and still take your pill. The kind where you cancel a hike because your knees scream, but you don’t stop living. Medicine gives us tools. But the real healing? That’s done by the person holding the pill bottle. Not the doctor. Not the trial. You.
I started on tamoxifen, switched to an AI after 3 years. My bone density dropped, but I got on denosumab. Now I hike again. It’s not perfect - but it’s mine. Also, I cry at commercials now. That’s new.
ai = joint pain
tamoxifen = uterine cancer risk
so… what’s the point again? oh right - we’re all just playing russian roulette with our hormones. cool. thanks science.
Per the 2023 ASCO guidelines, sequential therapy (tamoxifen followed by AI) is non-inferior to upfront AI in postmenopausal women. Duration should be individualized based on risk and tolerance.