Graves' disease: what to watch for and what to do
Graves' disease is an autoimmune cause of hyperthyroidism. Your immune system mistakenly turns the thyroid on too hard. That speeds up your body — heart races, you lose weight, you sweat more, and you may feel anxious or jittery. The good news: most people get better with proper treatment and follow-up.
Want straight answers? Here’s what matters most right now: how to spot it, how doctors confirm it, what your main treatment choices are, and simple everyday steps that really help.
Common signs and when to see a doctor
Look for fast heartbeat or palpitations, unplanned weight loss, heat intolerance, hand tremors, trouble sleeping, and more bowel movements. Women may have lighter or irregular periods. A firm swollen neck (goiter) is common. Eye changes — puffiness, redness, gritty feeling, or bulging — can happen and need special care.
Call your provider if you have chest pain, fainting, a very fast irregular heartbeat, very high fever, confusion, or severe vomiting. Those can be signs of thyroid storm, an emergency that needs immediate treatment.
How doctors confirm Graves' disease
Tests are simple. A blood test usually shows a low TSH and high free T4 or T3. Your doctor may check thyroid-stimulating immunoglobulin (TSI) to confirm Graves' disease specifically. Imaging like a thyroid ultrasound or a radioactive iodine uptake scan can help when the diagnosis is unclear.
Don’t be surprised if TSH lags behind symptoms. That’s normal — doctors often use free T4/T3 to adjust early treatment and check TSH later once things settle.
Treatment choices depend on your age, symptoms, pregnancy plans, and how active the eye disease is. Options are:
- Antithyroid drugs — methimazole is most common; propylthiouracil (PTU) is used in early pregnancy. These slow thyroid hormone production and can put the disease into remission for some people.
- Radioactive iodine — a pill that reduces thyroid function over weeks to months. It’s effective but often leads to permanent low thyroid function, which then needs lifelong thyroid hormone replacement.
- Surgery — removing part or all of the thyroid. It’s fast and useful when the gland is large, or when other options aren’t suitable.
Meanwhile, beta-blockers like propranolol can control heart rate and shakiness until other treatments take effect.
Eye problems (Graves' ophthalmopathy) may need a different approach: quitting smoking, artificial tears, steroids, or referral to an eye specialist for orbital treatments or surgery if vision is threatened.
Practical day-to-day tips: stop smoking, avoid high-dose iodine supplements, track heart rate and weight weekly, and keep follow-up blood tests as recommended. If you’re pregnant or planning pregnancy, tell your care team — treatment choices change during pregnancy.
Most people find a treatment that controls symptoms and lets them get back to normal life. If you’re unsure about a test or a treatment choice, ask for a clear explanation of risks and what follow-up will look like. That makes decisions easier and keeps you safer.
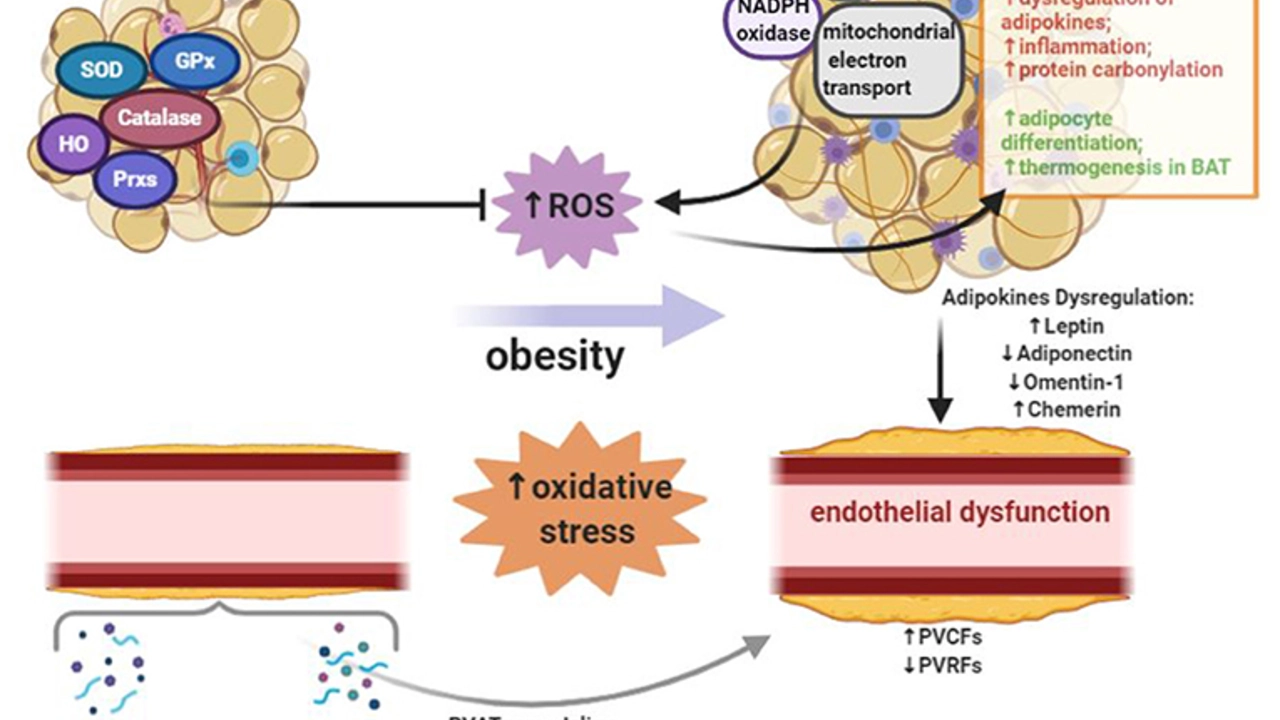
In my recent research on Graves' Disease, I discovered the crucial role that antioxidants play in managing this autoimmune disorder. As our body's defense mechanism against free radicals, antioxidants help reduce inflammation and oxidative stress, both of which contribute to the progression of Graves' Disease. By incorporating antioxidant-rich foods into our diet, such as fruits, vegetables, and whole grains, we can better support our immune system and overall health. Additionally, some studies suggest that antioxidant supplements may also be beneficial in managing symptoms. Overall, focusing on a diet rich in antioxidants could be a vital step in managing Graves' Disease and improving our quality of life.
Chris Gore Jun 18, 2023