Chronic Hepatitis C: what to watch for and what to do
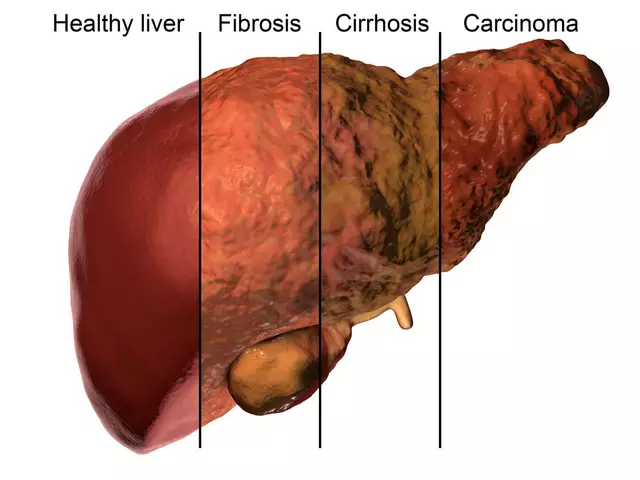
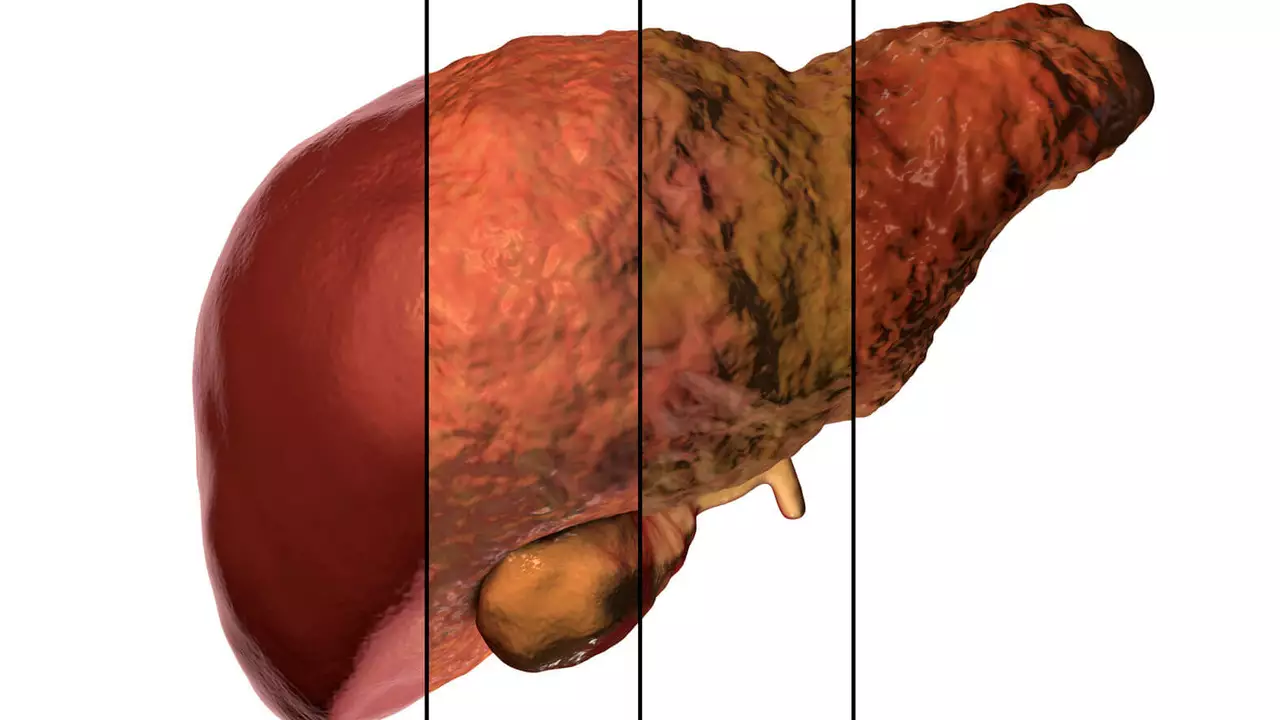
Chronic hepatitis C is a viral infection that damages the liver over time. Many people feel fine for years, so the first useful fact is this: you can have serious liver disease without obvious symptoms. That’s why testing matters if you had past exposure—like blood transfusions before 1992, shared needles, or long-term hemodialysis.
Diagnosis and modern treatment
Testing usually starts with an antibody blood test. If that's positive, your doctor orders an HCV RNA test to confirm active infection and measure viral load. You may also get liver blood tests (ALT, AST) and a scan or FibroScan to check fibrosis or cirrhosis.
Treatment changed everything. Direct-acting antivirals (DAAs) now cure most people—cure rates are over 95% for many common strains. These are oral medicines taken for 8–12 weeks in most cases. You need a prescription and follow-up blood tests to confirm the virus is gone (sustained virologic response). If you have cirrhosis or other health issues, your doctor will pick the best regimen and monitoring plan.
Daily care and prevention
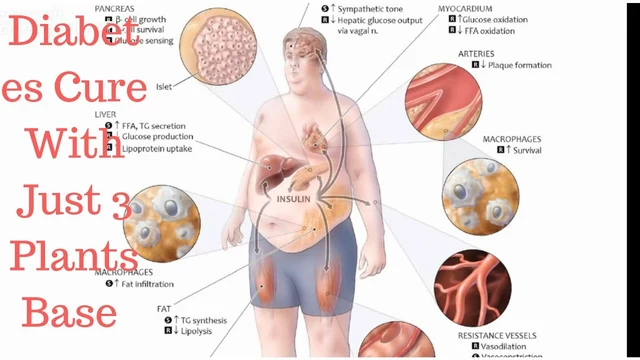
While on treatment, stick to the full course—missing doses can reduce success. Avoid alcohol and check any over-the-counter drugs with your clinician (acetaminophen in high doses can stress the liver). Get vaccinated against hepatitis A and B if you aren’t immune. Keep a healthy weight and control diabetes or high cholesterol—these lower added liver risk.
Prevent passing the virus: do not share needles, razors, or toothbrushes; cover open wounds; and talk with sexual partners about risks. Breastfeeding is generally allowed if nipples aren’t bleeding, but check with your provider. If you’re pregnant or planning pregnancy, discuss timing of treatment—some antivirals aren’t used during pregnancy.
People with advanced fibrosis need regular liver cancer screening—usually an ultrasound every six months. Even after a cure, follow-up depends on how much liver damage you had before treatment. Your healthcare team will set the right schedule.
Mental and emotional health matter too. A chronic diagnosis can trigger anxiety, depression, or isolation. Support groups, counseling, or patient networks can help you cope and stay on track with care. Many clinics also offer financial assistance or patient support programs to help cover treatment costs.
If you suspect exposure or have risk factors, get tested—early detection makes treatment simpler and more effective. Talk openly with your clinician about testing, treatment options, and practical daily steps to protect your liver and the people around you. Small actions—vaccines, avoiding alcohol, completing treatment—make a big difference.
Living with Chronic Hepatitis C can be quite challenging, but it's crucial to remember that self-care plays a significant role in managing the condition. Regular exercise, maintaining a balanced diet, and staying hydrated are key to keeping ourselves healthy. It's equally important to get regular check-ups and take our medication as prescribed. Mental health care is also vital, so seeking support from therapists or joining support groups can be very beneficial. Remember, taking care of our bodies is an act of self-love, and it's the first step in managing Chronic Hepatitis C.
Chris Gore Jul 1, 2023